When I was a child, I grabbed my father's pant leg in crowded areas to stay connected and safe. One day, I heard a very unfamiliar voice above, and I looked up to see that the man wearing the familiar trousers was certainly not my father. Trust was immediately replaced by fear and tension as I suddenly realized I was lost.
Healthcare leaders focus on critical metrics like health outcomes, staff retention, and financial performance. But what if I told you there's one element that dramatically influences all of these, including patient lifetime value?
Trust.
My childhood experience encapsulates the essence of trust in healthcare: it's fundamental, often unconscious, and when broken, can lead to fear and anxiety.
The neurobiology of trust
Let's start by looking at what happens in our brains when we experience trust. Trust is primarily mediated by a neurotransmitter called oxytocin. It's involved in bonding, social recognition, and yes, trust.
When we experience trust, our brains release oxytocin, which in turn activates specific neural pathways. This leads to a cascade of effects (The Neuroscience of Trust (hbr.org)):
- Reduced activity in the amygdala, our brain's fear center
- Increased activity in the nucleus accumbens, part of our reward system
- Enhanced connectivity between the insula, involved in interoception, and the anterior cingulate cortex, crucial for decision making
It's like a neural trust fall, except instead of potentially bruising your tailbone, you're creating the foundation for better health outcomes.
The staggering impact of trust in healthcare
Now, let's look at some numbers that made even my statistically-challenged brain do a double-take:
Consider these striking statistics:
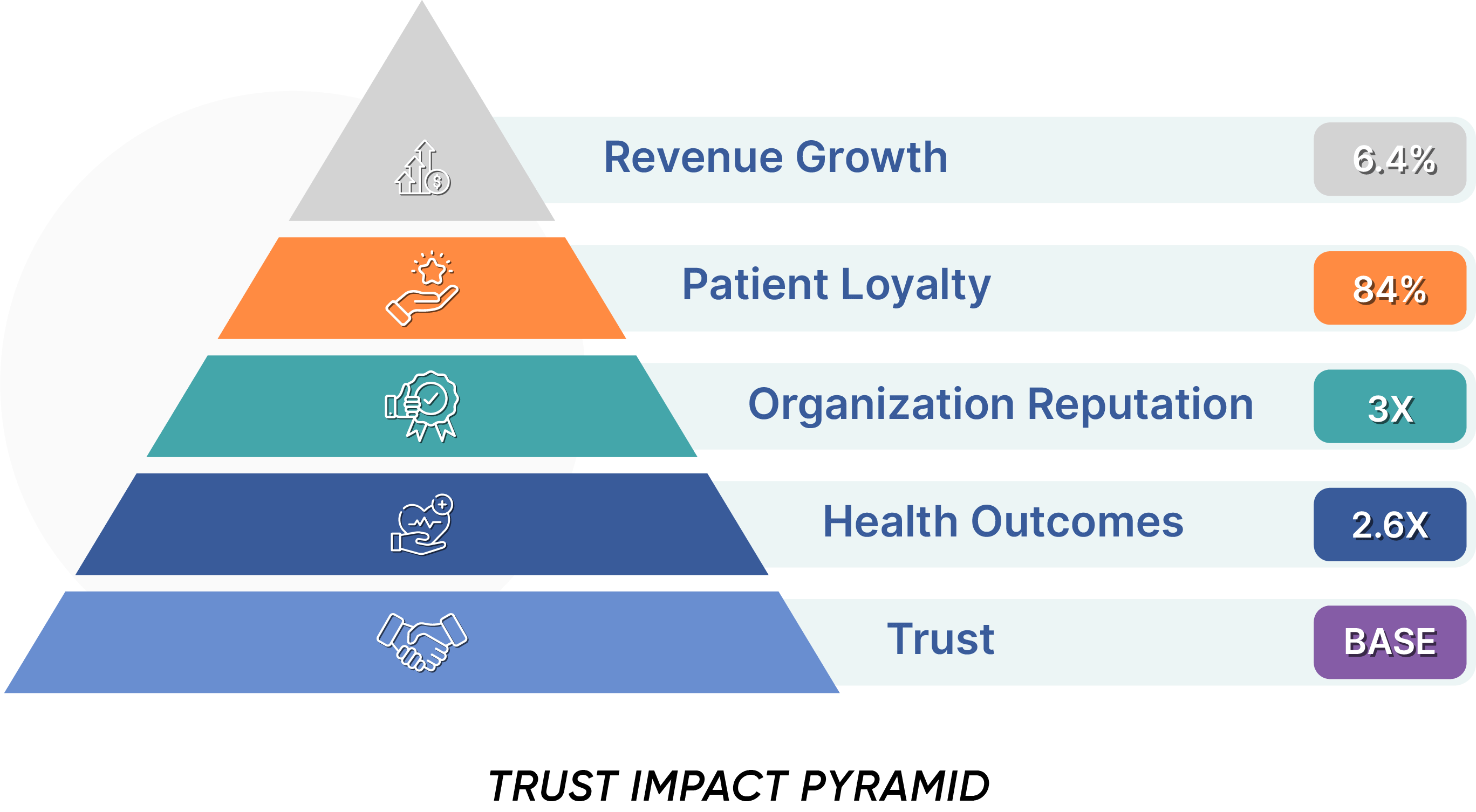
- Patients with high trust in their healthcare providers are 2.6 times more likely to adhere to treatment plans (NCBI Article on Trust and Adherence).
- Healthcare organizations with high levels of customer trust outperform their peers by 6.4% in revenue growth (PLOS ONE).
- Patients with high trust levels are 3 times more likely to recommend their healthcare provider (NCBI Article on the Development of a Trust Scale).
For over 30 years researchers have recognized the essential role that trust plays in healthcare outcomes. These numbers paint a clear picture: trust isn't just a feel-good concept—it's a powerful driver of healthcare excellence and organizational success. It's the foundation of what we might call "trust-driven greatness," where every interaction, decision, and outcome is rooted in the deep trust your stakeholders place in your organization.
The neurochemistry of patient-centered care
Now, you've probably heard buzzwords like "patient-centered care" and "patient experience" thrown around more often than I use the word "fascinating."
The common thread tying these concepts together? Trust.
When a patient trusts their healthcare provider, several key things happen in their brain:
- Oxytocin release increases, promoting bonding and reducing stress
- Cortisol levels decrease, lowering overall stress and inflammation
- The prefrontal cortex, responsible for decision-making and impulse control, becomes more engaged
This neurochemical cocktail creates an environment where patients are more likely to:
- Openly communicate about their symptoms and concerns
- Adhere to treatment plans
- Engage in preventive care
- Feel satisfied with their care
It's like giving your brain a trust supplement, except unlike most of the supplements I've tried, this one actually has solid scientific backing.
Let's dive into the critical questions that can guide your path to trust-driven greatness:
Why is trust Important in healthcare?

Gina Tabone, MSN, with over 25 years of experience from Cleveland Clinic to consulting, emphasizes the importance of trust:
"Research shows if your employees trust your organization and your leadership, that will come across when they speak to your patients. Trust-driven greatness is really about putting the needs of the patient first and making every single interaction meaningful."
Health outcomes: Trust is the foundation of effective patient-centered care. Studies show that patients with higher levels of trust in their healthcare providers are **2.6 times more likely** to adhere to their treatment plans(NCBI Article on Trust and Adherence). This staggering 160% improvement in adherence directly impacts health outcomes.
According to a study published in the Journal of General Internal Medicine, higher levels of patient trust in their healthcare providers are associated with:
- Improved health outcomes
- Higher likelihood of seeking preventive care
- Increased patient satisfaction
- Greater patient engagement
(PDF) Trust in the health care professional and health outcome: A meta-analysis (researchgate.net)
Trust also fosters open communication, making patients more likely to share important information that can impact their care.
Patient Loyalty: Trust is also a driver of loyalty and patient lifetime value. Surprisingly, one study reveals that trust is more important than satisfaction in fostering patient loyalty in private healthcare settings. While patient satisfaction is necessary, it does not directly translate into loyalty unless it leads to trust. (NCBI Article on the Development of a Trust Scale)
Organizational Reputation: A strong reputation for trust attracts patients, partners, and top talent. Word of mouth - A study by the Beryl Institute found that patients with high trust levels are 3 times more likely to recommend a healthcare provider. (PXPulse_Sept2021-8bcotp.pdf (theberylinstitute.org)) A study by Edelman found that trust is the most important factor in determining a company's reputation (Trust Surges to Become the Second Most Important Purchasing Factor for Brands | Edelman).
Revenue Growth: Given the above, it should be no surprise that financial performance is also a benefit. A report by Accenture found that healthcare providers with high levels of customer trust outperform their peers by 6.4% in terms of revenue growth. (Healthcare Technology Trends 2022 | Tech Vision | Accenture)
Whose trust is important?
Case Study: Cleveland Clinic’s TransformationThe Cleveland Clinic, once perceived as an elitist institution disconnected from its inner-city community, underwent a significant transformation by focusing on trust and community engagement. Under the leadership of CEO Toby Cosgrove, the Clinic centralized and standardized services, particularly emphasizing access to care. This involved empowering staff through focus groups, engaging them in decision-making, and aligning initiatives with the Clinic’s mission of patient-centered care. The result was a cultural shift that not only improved employee morale but also significantly enhanced patient trust and satisfaction. |

Trust is vital across multiple relationships in healthcare:
- Patient trust in physicians Trust is vital across multiple relationships in healthcare. is crucial for ensuring adherence to medical advice and maintaining patient loyalty.
- Patient trust in the healthcare team Furthermore, patient loyalty is driven more by the entire team than by the provider. An Accenture study found that a negative provider experience only contributed to 44% of patients leaving, but difficulty with the office, communication, and online contributed to 89% of patients who switched (Health-Provider-Loyalty-Accenture.pdf).
Deloitte research found that 55% of study participants experienced negative healthcare interactions leading to a significant loss of trust – and these were often not with the provider (Rebuilding trust in health care | Deloitte). This underscores the truth that ALL service is care, whether by the provider or any team member.
“ALL service is care, whether by the provider or any team member.”
- Clinician trust in their organizations is essential for creating a positive work environment, which directly impacts provider satisfaction and the quality of care provided to patients (Assessing Trust in Health Care: A Compendium of Trust Measures | AcademyHealth).
- Internal trust among staff Gallup's State of the American Workplace report consistently highlights the correlation between trust and employee engagement (State of the Global Workplace Report - Gallup).
Fostering a culture of transparency and collaboration within the healthcare organization can improve clinician trust, which in turn enhances patient trust. Cindy Feeley, a healthcare call center consultant, highlights the importance of consistency in building trust:
"Inconsistent handling confuses staff and patients alike... This internal lack of trust unavoidably flows right into poor patient service."
What is the largest factor in trust & loyalty?

When you get into the passenger seat of a car, you are placing a significant amount of trust in the driver. You trust that they will follow the rules of the road, navigate safely, and make decisions that protect both of you. Most people don’t consciously think about this trust, but it’s an inherent part of the experience. If you didn’t trust the driver, you would feel anxious, tense, and constantly on edge, second-guessing every move they make.
However, when trust is present, you can relax, enjoy the ride, and focus on other things, knowing that you’re in safe hands. This analogy perfectly encapsulates the patient-provider dynamic—when patients trust their providers to navigate the complexities of healthcare, they can focus on healing and recovery.
Accenture’s extensive survey found the largest factor influencing trust and loyalty for the patient is what is called the patient experience:
- Ease of patient access
- Clear communication
- Digital engagement
Accenture’s research highlights that patients who find their providers easy to work with are 84% more likely to stay with them (Health-Provider-Loyalty-Accenture.pdf).
A systematic review published in PLOS ONE was focused on the provider relationship specifically, and it found that effective provider-patient communication was the most significant factor in building and maintaining trust Building trust and rapport early in the new doctor-patient relationship: a longitudinal qualitative study - PMC (nih.gov)
"Confidence is sort of a byproduct of trust," added Gina Tabone. "When patients have better experiences, trust is already there. It's really an action term—it's a lot of work, but if you always keep the patient at the core of what you're doing, your propensity for success is greater."
What can I do to improve trust?
To truly enhance trust and achieve patient-centered care, healthcare organizations need to adopt a systematic approach to improving the patient experience. This process begins with understanding patient needs and extends to creating unified, efficient workflows across departments.
Case Study: Cindy Feeley’s Trust-Driven TransformationCindy Feeley, a seasoned healthcare service expert, led a trust-driven transformation at a large medical group plagued by patient complaints and operational inefficiencies. By centralizing the call center and focusing on improving first contact resolution, Feeley not only reduced patient frustration but also saw an 11% increase in shown appointments—far exceeding the 1% needed to justify the investment. Her approach, rooted in aligning the entire team around trust and service excellence, led to significant improvements in patient satisfaction, revenue, and the organization’s reputation. Cindy Feeley's perspective on trust-driven greatness: "Trust driven greatness to me is really making sure that you are constantly driving forward in delivering the best excellence in customer service that you can. Knowing that this will ultimately drive your business to be the best it can be. It's a constant journey of improving the service that you're delivering to your patients." |
Let's break down this approach:
 Align organizational mission with patient experience
Align organizational mission with patient experience
-
- Review or Reiterate the Mission Statement: Most healthcare companies will explicitly reference patient care or patient experience as core reasons for the organization's existence.
- Communicate the Mission: Ensure that all employees, from frontline staff to executives, understand and can articulate how their role contributes to the patient-centric mission.
- Align Strategic Initiatives: Ensure that all major initiatives and decisions are evaluated against their impact on patient experience and trust-building.
- Lead by Example: Leadership should consistently demonstrate commitment to the patient-centric mission in their decision-making and communications.
 Audit all patient touchpoints
Audit all patient touchpoints
- The foundation of improving patient experience lies in comprehensively understanding all types of patient interactions. A study by Accenture found that 26% of patients have switched healthcare providers due to poor customer experience(Today's Consumers Reveal the Future of Healthcare | Accenture). This makes it crucial to:
- Conduct a Touchpoint Audit: Map out every interaction patients have with your organization, from initial contact to post-treatment follow-ups.
- Use Patient Journey Mapping: Visualize the entire patient experience to identify pain points and areas for improvement.
- Engage in Continuous Feedback Loops: Regularly gather feedback from patients at each touchpoint to refine and improve the experience.
 Centralize & optimize patient service operations
Centralize & optimize patient service operations
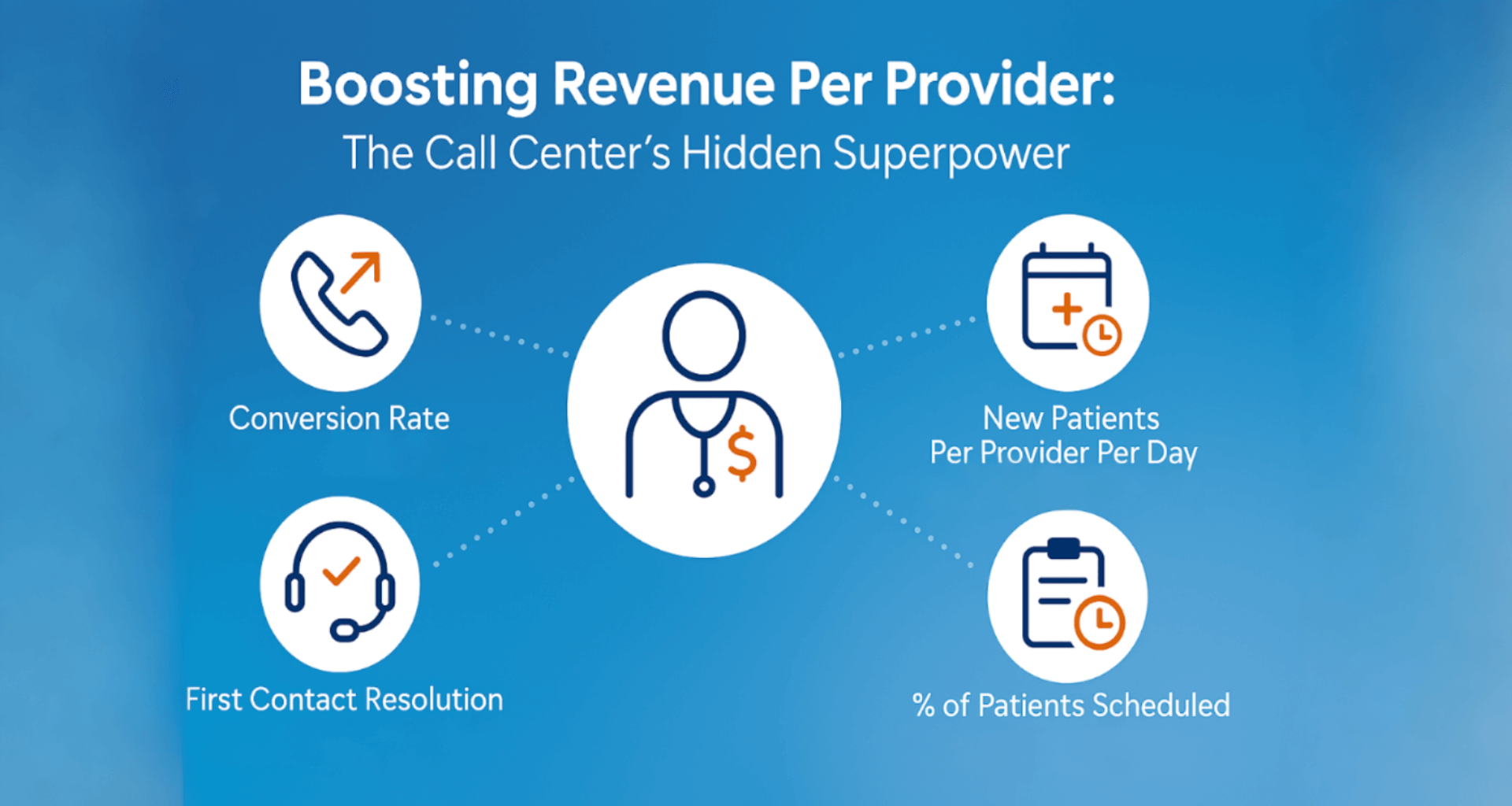
The call center and front desk often serve as the hub of patient interactions. According to a survey by Healthcare Call Center Times, 70% of patients form their impression of a healthcare organization based on their experience with the call center (Healthcare Call Center Times. (2020). "The Role of Call Centers in Patient Experience."). To optimize these crucial touchpoints:
-
- Implement a Healthcare CRM System: a healthcare customer relationship management (CRM) system is the central nervous system of patient interactions. It streamlines communication and service delivery while aggregating all data on patient interactions.
- Develop Standardized Call Flows: Create and train staff on standardized call scripts and procedures to ensure consistent and high-quality service.
- Focus on Empathy Training: Invest in training programs that enhance the empathetic communication skills of all employees.
Golden State Orthopedics Case StudyGolden State Orthopedics & Spine (Golden State), a large orthopedic practice with over 75 providers, faced challenges with high call volumes, long hold times, and inconsistencies in scheduling due to their fragmented call center operations. By implementing CareDesk, a healthcare CRM, Golden State centralized and optimized their patient service operations, reducing training time by 75%, increasing call handling capacity by 125%, and significantly improving scheduling accuracy. This transformation not only enhanced patient access but also allowed the practice to integrate a cost-effective, offshore call center, further improving efficiency and reducing operational costs. The success of this initiative was driven by strong executive sponsorship, thorough configuration of scheduling protocols, and seamless EMR integration, setting GSOS as a model for other large specialty practices looking to streamline their operations and improve patient satisfaction. |
 Collect and Analyze Service Data
Collect and Analyze Service Data
Data-driven decision making is crucial for continuous improvement. A report by McKinsey found that healthcare providers using advanced analytics to improve patient experience saw a 10-15% increase in patient satisfaction scores (The big-data revolution in US health care: Accelerating value and innovation | McKinsey). Key steps include:
-
- Leverage Data Analytics Tools: Use analytics platforms to track key service metrics like appointment conversion, first-call resolution, and patient satisfaction.
(get the ebook: 15 Most Important Patient Experience Metrics) - Establish Regular Reporting Cycles: Create a routine for analyzing and sharing service performance data with relevant teams.
- Implement Continuous Improvement Programs: Use insights from data analysis to drive ongoing improvements in patient service operations.
- Leverage Data Analytics Tools: Use analytics platforms to track key service metrics like appointment conversion, first-call resolution, and patient satisfaction.
 Unify Departments with Patient-Centric Workflows
Unify Departments with Patient-Centric Workflows
Siloed departments can lead to fragmented patient experiences. A study in the Journal of Healthcare Management found that cross-functional teams improved patient satisfaction scores by 18% and reduced wait times by 25% (Smith, J. et al. (2019). “Impact of Cross-Functional Teams on Patient Experience.” Journal of Healthcare Management, 64(1), 23-35.).
To achieve this:
-
- Create Cross-Functional Teams: Develop teams that include members from different departments focused on improving specific aspects of the patient journey.
- Standardize Communication Protocols: Ensure all departments use the same communication protocols to avoid confusion and miscommunication.
- Establish Shared Goals: Align departmental goals with patient-centric outcomes, ensuring that everyone is working towards the same objectives.
- Foster Personal Development Across Roles: Healthcare organizations can sometimes make the mistake of inadvertently making many of the non-clinical jobs dead-end, without a path for recognition and promotion. To combat this, take an active role in developing all employees into their next roles, including both investment in training and clear paths for promotion.
 Unify Your Service Tech Stack
Unify Your Service Tech Stack
A unified technology approach can significantly improve efficiency and consistency. Key steps include:
-
- Conduct a Technology Audit: Review your existing tech stack to identify redundancies, gaps, and opportunities for integration.
- Integrate Systems for Seamless Experience: Ensure that all patient-facing technologies (e.g., EHR, patient portals) are fully integrated for a seamless experience.
- Prioritize User Experience: Optimize the user interface of all patient-facing technologies to ensure ease of use and accessibility.
 Build Automation Around Frequent Services
Build Automation Around Frequent Services
Automation can improve consistency and free up staff time for more complex patient needs. Consider:
-
- Implement Chatbots for Routine Inquiries: Use AI-powered chatbots to handle common patient questions and appointment scheduling.
- Automate Back-Office Tasks: Introduce automated tools to handle repetitive administrative tasks to free up staff for more critical duties.
- Set Up Automated Follow-Ups: Develop systems that automatically send appointment reminders, follow-up surveys, and post-visit care instructions.
 Continuously Measure and Improve
Continuously Measure and Improve
Achieving trust-driven greatness is an ongoing process. To maintain momentum:
-
- Establish KPIs for Patient Experience: Define and track key performance indicators (KPIs) related to patient trust, satisfaction, and service quality.
- Conduct Regular Surveys and Focus Groups: Gather patient feedback through surveys and focus groups to identify areas for improvement.
- Celebrate and Learn: Recognize successes in improving patient experience and learn from any setbacks to foster a culture of continuous improvement.
The role of leadership in this process cannot be overstated. As Gina Tabone notes:
"Executive leadership is about setting expectations and modeling those critical behaviors that make patient experiences feel less like a maze and more like a well-guided tour. It's about actions that convey trust, bringing in all the key players and ensuring that everyone knows their role in the patient care process."
Patient Journey Maturity Model
Healthcare organizations often struggle with fragmented patient service across multiple touchpoints. The Patient Service Maturity Model by Keona Health is a strategic framework designed to guide organizations from foundational practices to scalable excellence. By leveraging consistent standards, advanced automation, and omnichannel engagement, this model empowers your team to deliver high-quality care while driving efficiency and growth. Assess your organization today to start transforming patient service. |
By systematically implementing these strategies and embracing the philosophy of trust-driven greatness, healthcare organizations can create a patient experience that fosters trust, improves outcomes, and drives organizational success. As Cindy Feeley reminds us:
"If the company is focused on delivering greatness to their customer or patient base, they're the ones that ultimately wind up succeeding. Trust-driven greatness means you're on a journey where you should always be improving."
Remember, this is not a one-time effort but an ongoing commitment to putting patients at the center of everything you do. The path to trust-driven greatness in healthcare is challenging, but the rewards—in terms of patient outcomes, satisfaction, and organizational success—are immeasurable.
For more information on implementing these strategies, including Patient Experience Steering Committee checklists, videos, and eBooks on Patient Service Metrics, visit Learning Resources.
Posted By

Stephen Dean is COO of Keona Health, where he’s spent 13 years building AI systems that transform patient access. Before “agentic AI” was a term, his team was deploying autonomous systems that now handle millions of patient conversations annually.
Related Post
July 30, 2025
when patients call, they’re not just dialing a number—they’re reaching for help. and...
April 10, 2025
in healthcare, every interaction is a decision point—one that can impact outcomes,...