In healthcare, every interaction is a decision point—one that can impact outcomes, satisfaction, and the financial health of your practice. And in the contact center, those decisions come fast and often without a full picture.
It’s a little like being a triage nurse in the dark. Except instead of vitals and symptoms, you're juggling handle times, routing issues, and appointment slots… all while trying to help someone you’ve never met feel cared for, understood, and guided to the right next step.
That’s why one metric—Revenue Per Provider (RPP)—has become a quiet but powerful north star.
Why Revenue Per Provider Belongs on Your Dashboard
RPP isn’t just a finance department number. It’s the signal that your contact center is doing more than answering phones—it’s guiding people to care that matters, when it matters.
Think of it as the financial reflection of patient access. By aligning your patient acquisition, scheduling, and support workflows, you not only increase Revenue Per Provider—you reduce inefficiencies across the entire access funnel.
When your workflows are smooth, your scheduling is smart, and your staff is empowered, RPP goes up. When patients bounce around from agent to agent, or fall through the cracks of a clunky system, it goes down.
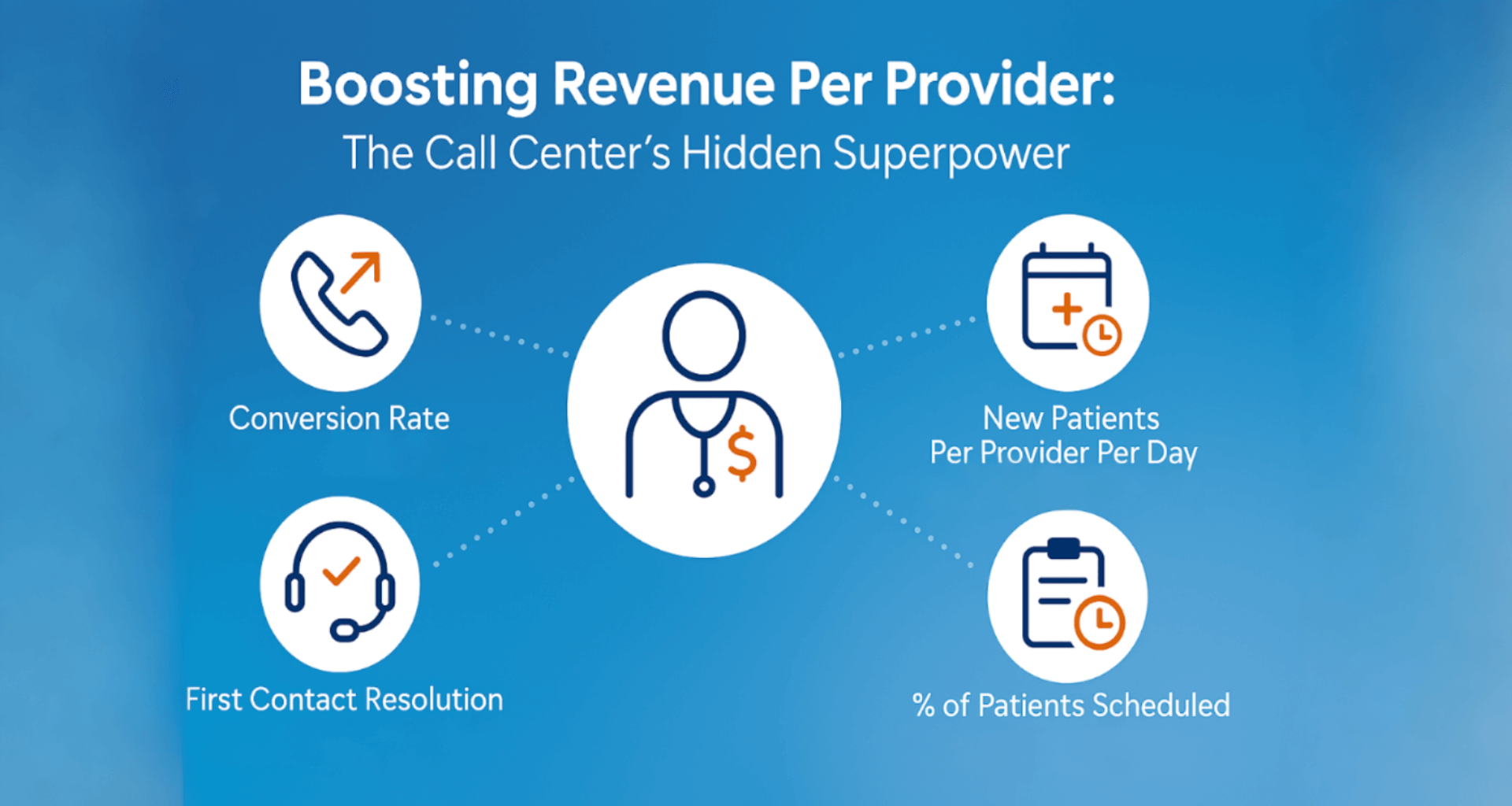
How To Boost Revenue Per Provider
So how do we move that number in the right direction—without turning your team into robotic schedulers? Here are 4 supporting metrics and practical tips for each one:
 Conversion Rate:
Conversion Rate:
Your Window into Missed Opportunity
If your contact center handles 10,000 calls a month, but you don’t know how many result in scheduled care… you're flying blind.
The goal isn’t to push more appointments. It’s to recognize when someone needs care and guide them there effectively.
Let’s bring this home:
An agent who converts 10% of appropriate calls into appointments adds more value than someone flying through twice the volume at 5%. But unless you're measuring that conversion, you won’t know the difference.
Take Jen, one of your best performers—at least on paper. Fast calls, high volume, glowing dashboards. But when you dig into the data, you see that Jen’s patients are far less likely to schedule. She’s so focused on moving to the next call, she’s missing the real opportunity: helping the patient in front of her.
Ways to Boost Conversions—Without Pushing:
- Balance metrics: Speed isn’t everything. If your scorecard rewards fast calls but not outcomes, you might be optimizing for abandonment.
- Real-time decision support: Equip agents with dynamic guides that recommend the right services for the caller’s need.
- Cut the handoffs: Every transfer is a chance for the patient to give up. First-contact resolution isn’t just efficient—it’s compassionate.
Kaufman Hall’s 2023 research shows that nearly one-third of healthcare leaders saw rising patient complaints about access—while more than half struggled to meet demand. Access is a major patient experience issue with real consequences for loyalty, satisfaction, and financial performance.
Metrics like conversion rate aren’t “sales-y”—they’re care-quality indicators in disguise.
 New Patients Per Provider Per Day:
New Patients Per Provider Per Day:
Measuring Front Door Growth
Growth doesn’t just happen—it walks in … through the call center.
Tracking new patients per provider per day gives you a realistic view of whether your outreach and intake are working, month over month. And yes, “per day” matters—because a 22-day month is very different from an 18-day one.
But behind that number is something deeper: a story of trust.
When someone calls unsure, nervous, or frustrated—and your team makes them feel seen and supported—you’re doing more than filling a slot. You’re welcoming someone into long-term care.
Three things that help:
- Agent-as-advocate mindset: Train staff to listen actively, empathize quickly, and be problem-solvers—not script-readers.
- Intelligent scheduling: Use smart systems that match patients with providers based on needs, availability, and even preferences.
- Follow-up that feels human: Automated reminders shouldn’t sound robotic. Use them to gently keep your name top of mind for patients who weren’t ready today.
 First Contact Resolution (FCR):
First Contact Resolution (FCR):
Your Hidden Efficiency Engine
FCR isn’t just a contact center metric—it’s a patient experience milestone.
Every time a patient has to call back to resolve an issue, it’s a trust withdrawal. Each successful resolution in a single call? That’s a deposit in the loyalty bank.
Take Ellen. She’s called twice this week, trying to reschedule an appointment after her transportation fell through. She’s explained her story twice, waited on hold twice, and still doesn’t have her issue resolved. Meanwhile, there are open provider slots tomorrow. That’s a preventable failure—but only if you're tracking FCR.
In practical terms, better FCR means shorter total call volumes, happier staff, and fewer missed care opportunities.
Tactics that work:
- Equip call center staff to solve problems—check eligibility, schedule directly, resolve common issues.
- Automate administrative friction (reminders, automation, and self-service).
- Track the right data: Resolution isn’t always obvious in call logs—tie tasks to outcomes.
According to a Calabrio case study, improving FCR led to a 20% increase in resolution success and a 40% drop in both customer effort and error rates—proof that when patients don’t have to keep calling, everyone wins.
 Percentage of Patients Scheduled:
Percentage of Patients Scheduled:
Closing the Loop on Demand
Every open slot is a silent alarm. It’s not just lost revenue—it’s a patient who didn’t get care.
Online scheduling and self-service options help, but they don’t fix everything. The real win is designing systems that reduce friction and give patients multiple ways to engage, with consistent results.
Also—let’s be honest. In healthcare, we’re data hoarders. We collect so much info, but sometimes the things that actually matter—like how many eligible patients didn’t schedule—get lost in the clutter. Time to bring that to the surface.
The Big Idea: Growth Without Burnout
Let’s say it clearly—improving RPP isn’t about doing more with less. It’s about doing the right things better. True healthcare revenue cycle improvement isn’t about squeezing more out of your team—it’s about creating workflows and tools that unlock their full value.
That’s how you deliver care with heart and precision. That’s how you build a system that improves healthcare financial performance while supporting providers and patients alike.
Ready to improve Revenue Per Provider?
Start small. Pick one metric you’re not tracking—or not using well—and dig in. The future of your access operations isn’t just about faster—it’s about wiser, stronger, and more sustainable.
The kind of future your patients and staff both deserve.
Posted By

Stephen Dean is COO of Keona Health, where he’s spent 13 years building AI systems that transform patient access. Before “agentic AI” was a term, his team was deploying autonomous systems that now handle millions of patient conversations annually.
Related Post
July 30, 2025
when patients call, they’re not just dialing a number—they’re reaching for help. and...

