The truth about measuring patient satisfaction
Sarah, a call center supervisor, was part of a cross-functional team tasked with finding answers about declining patient retention. She found herself staring at yet another spreadsheet of patient satisfaction data. The numbers blurred together like highway lines on a rainy night. Despite mountains of metrics, Sarah couldn't see the forest for the trees. "I have all this data," she said, "but I still can't tell my leadership team why patients aren't coming back."
Sarah's story is common. You likely grapple with patient data without gaining insights. We've all tried to decode numbers that don't reflect real experiences.
The Data-Rich, Insight-Poor Paradox
Here's the truth: 81% of healthcare executives prioritize patient experience, but only 11% understand patient retention, per ConvIQ. It's like having a map but no sense of direction.
Healthcare leaders cling to annual HCAHPS surveys as lifelines, hoping they lead to patient satisfaction. We monitor call volumes and abandonment rates, mistaking these metrics as the full picture.
Once, a patient, Miguel, called his provider three times for a prescription issue. "My survey only asked if my call was answered promptly," he says. "No one checked if my problem wass fixed." The numbers show his experience as excellent, but his reality differed.
Three Misconceptions About Measuring Patient Experience
Misconception #1: HCAHPS surveys are enough.
Imagine guessing what your spouse wants for your anniversary based on last year's comments. That's the flaw of relying solely on annual HCAHPS surveys. They offer snapshots from a limited patient sample. The 2023 Healthcare Experience Trends Report by Qualtrics underscores that personal connections, not just efficiency, win loyalty. Empathy in service boosts satisfaction. Two-thirds (63%) of consumers think companies must improve listening.
Misconception #2: Surface-level call center metrics show the whole picture.
Judging a meal by its speed is like obsessing over call volume and abandonment rates without deeper analysis. These metrics should pair with patient sentiment, effort, and loyalty throughout the healthcare journey. Poor communication, a leading cause of medical errors, harms patients. Effective provider communication prevents errors, enhancing safety and satisfaction.
Chausa reports that Poor communication is identified as a leading cause of medical errors, which can result in adverse events and patient harm. Effective communication among healthcare providers is crucial for preventing avoidable outcomes and promoting patient safety, thereby enhancing patient satisfaction.
Misconception #3: Checking the compliance box is sufficient.
Think of a "clean" hotel where the experience lacks. That's the compliance vs. excellence difference. Meeting minimum standards avoids trouble but doesn't boost satisfaction or provide patient-centered care. Patients now expect more than basic service; they want effortless, personalized care, and value in every interaction. A McKinsey study finds 70% of buying experiences rely on perceived treatment.
The Holistic Approach: Measure What Matters
Remember Sarah? Three months after adopting holistic patient metrics, she feels different at the morning meeting. "Patients who take multiple calls to resolve their issue are three times likelier to switch providers in six months," she says. "We've improved first call resolution by 30% and increased retention by 12%."
Transformation means a holistic, actionable evaluation of patient experience. Track the right metrics to understand what's happening, why, and how to change it.
Experts at the Harvard T.H. Chan School of Public Health link performance measurement systems, including patient experience metrics, to better financial outcomes. These systems aid the Triple Aim: enhancing health, reducing costs, and improving experiences.
15 essential patient experience metrics every healthcare call center should be tracking
Instead of bombarding you with an overwhelming list, let's explore some key metrics by category and why they matter to the people behind the numbers:
Forward Looking Metrics:
- Net Promoter Score (NPS) – The ultimate question of loyalty
- New patients this week/month – Your growth barometer
- Customer Effort Score (CES) – How easy are you making healthcare?
Backward Looking Metrics:
4. Revenue Growth – The financial pulse of patient satisfaction
5. # Unique patients / month – Your retention reality check
Operations Metrics:
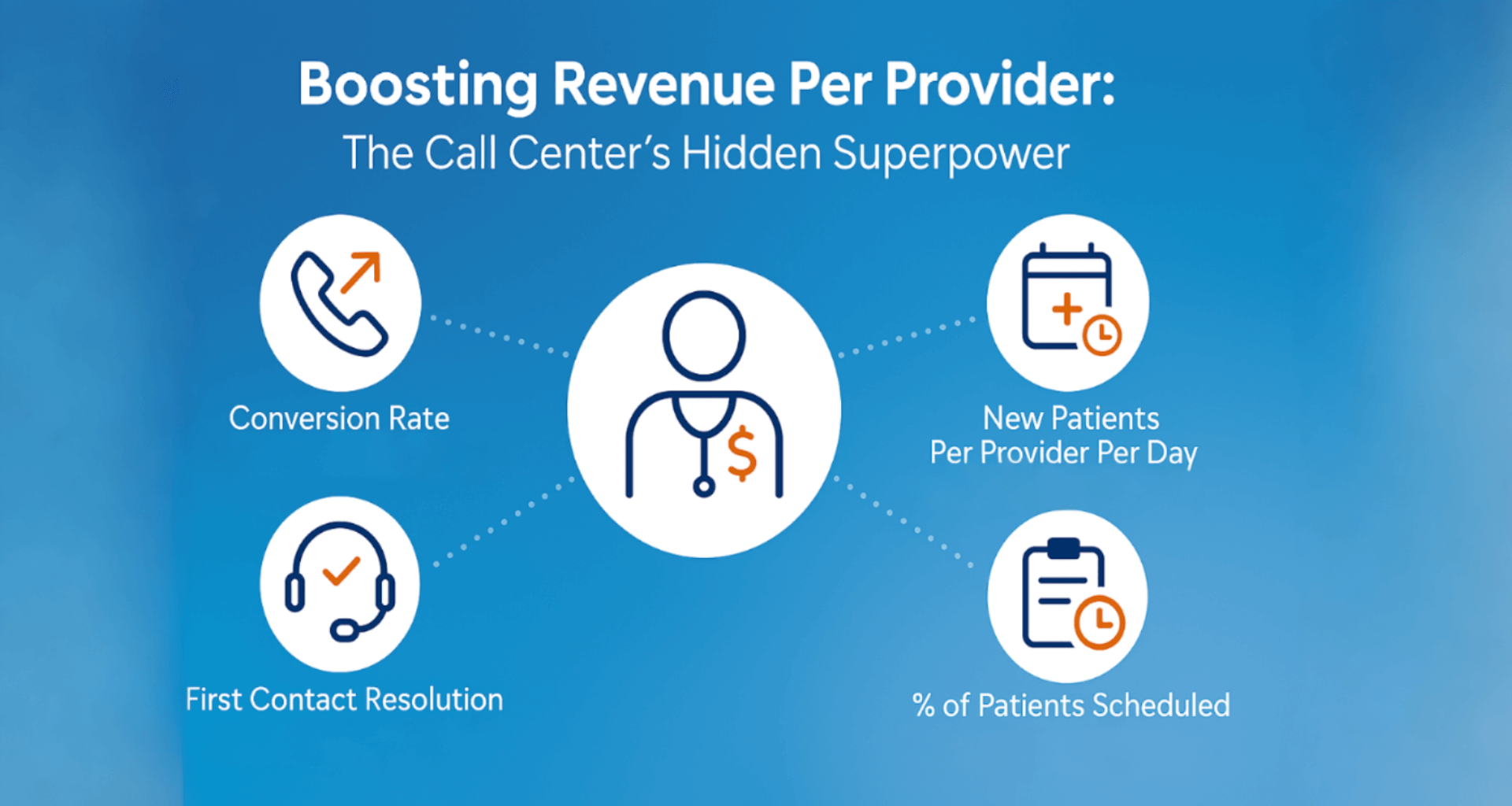
6. First Contact Resolution (FCR) – One and done, or frustration begun?
7. Time to Resolve – The patience clock is ticking
8. Employee Satisfaction – Happy staff, happy patients
9. % new patients scheduled / total call handled per patient – Your conversion reality
10. Quality scores– Beyond the checkbox
Contact Reaction Metrics:
11. Average speed of answer – First impressions matter
12. Abandonment rate– The silent exodus
13. Service level– Promises kept or broken
Efficiency Metrics
14. Average Handle Time (AHT) – Balance speed with care
15. Adherence Rate – The reliability factor
Let's Dive Deeper: The Metrics That Move the Needle
Download our free eBook: "The 15 Most Important Patient Experience Metrics"
Let's examine some of these patient experience measures and why they matter so much.
Net Promoter Score (NPS): : The Ultimate Loyalty Predictor
Widely considered one of the most important patient experience metrics, NPS is your healthcare's friendship measure. Based on "How likely are you to recommend our services?" responses are promoters (9-10), passives (7-8), or detractors (0-6). Subtract detractors' percentage from promoters' percentage for your NPS.
Emma, a Denver practice manager, improved her clinic after noting detractor scores from booking issues. "Patients love our doctors but hate our system," she says. "Addressing our top 3 booking complaints raised our NPS from 23 to 62 in six months."
Customer Effort Score (CES): Simplicity in Healthcare
"I just want it easy," Tony, a 72-year-old scheduling his follow-up, says. CES measures ease (or difficulty) of resolving issues. Studies show CES predicts loyalty. A low-effort experience boosts satisfaction and retention, proving simplicity predicts loyalty even more than delighting patients.
To calculate CES, simply ask patients, "How easy was it to get your issue resolved today?" on a scale of 1 (very difficult) to 5 (very easy). Address "difficult" responses and identify effort-increasing patterns.
First Contact Resolution (FCR): One and Done
Remember playing "hot potato" as a kid? In healthcare call centers, patients often feel like they're the potato—passed from person to person without resolution. FCR tracks the percentage of patient inquiries resolved on the first interaction, without callbacks, transfers, or escalations.
Arguably the most important operational metric for healthcare call centers, a high FCR creates a triple win: patients get answers quickly, staff feel more effective, and your organization handles fewer repeat contacts. Aim for at least 80% FCR, with best-in-class organizations achieving 95% or higher.
Employee Engagement: the Foundation of Patient Experience
Maria had been answering calls at her healthcare system for seven years. When asked why she stayed while others left, she said simply, "They make me feel like what I do matters. And because it matters to them, it matters more to me."
Your staff are not just the face of your healthcare brand—they're its heart. If they're disengaged, burnout seeps through the phone lines. Gallup found that healthcare organizations with highly engaged teams outperform their peers by 147% in earnings per share.
Financial impact: Satisfaction and Revenue
Key metrics like patient churn rate and lifetime value can help you quantify the ROI of your improvement efforts and make the case for further investment. For example, a study by Accenture found that U.S. hospitals that provide "superior" patient experiences generate 50% higher financial performance than "average" health care providers do.
Never stop refining your patient satisfaction efforts
Patient experience improvement isn't a destination—it's an ongoing journey. It requires sustained commitment from leadership, a willingness to experiment (and sometimes fail), and a relentless focus on patient needs and preferences.
Start by sharing your metrics with your entire team. Celebrate the wins, learn from the setbacks, and never stop listening to your patients.
In a healthcare landscape where patients have more choices than ever, exceptional experience isn't optional—it's essential for survival and growth.
Learn more by downloading our free 37-page eBook: "The 15 Most Important Patient Experience Metrics"
Posted By

Stephen Dean is COO of Keona Health, where he’s spent 13 years building AI systems that transform patient access. Before “agentic AI” was a term, his team was deploying autonomous systems that now handle millions of patient conversations annually.
Related Post
July 30, 2025
when patients call, they’re not just dialing a number—they’re reaching for help. and...
April 10, 2025
in healthcare, every interaction is a decision point—one that can impact outcomes,...