Intro
Telehealth is undergoing a sea of change in medical delivery. Long-distance clinical health care solutions can be hard to stand-up, especially for rural providers already stretched thin due to large coverage areas. Healthcare service delivery and healthcare team devices are critical for remote healthcare services and behavioral healthcare services.
You may be ready for a full telehealth platform, or maybe you simply want to add a single offering as a telehealth service. Either way, your telehealth strategy should be holistic – including everything you need to improve workflows: break down old silos & deliver better outcomes with less overhead. Keep reading for a comprehensive overview covering essential topics ranging from essential costs and reimbursement considerations to staff & telehealth provider training tips & more!
When most people think of telehealth, they think only of a provider visit over video chat. This is actually called Telemedicine, and you can read more about HIPAA compliant telemedicine below. Telehealth, on the other hand, is far, far more. So what exactly is Telehealth then?
Luckily, a department inside of the U.S. Department of Health and Human Services (HHS) has already defined Telehealth for us.
What is Telehealth?
"Any use of electronic information and telecommunications technologies to support and promote long-distance clinical health care, patient and professional health-related education, and public health and health administration." -Health Resources and Services Administration (HRSA)
This is far-reaching! Basically, any use of digital technology to provide services to patients over a distance is part of telehealth.
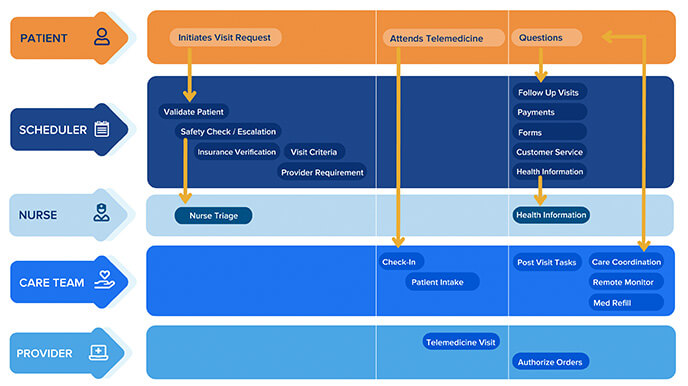
But what does that mean, really? Let’s start with an overview of all the telehealth services provided in a typical single-visit process:
Typical Services Required for holistic Telehealth delivery:
- Scheduling visits
- Provide nurse triage and health information
- Telemedicine visits
- Medication refill
- Patient intake
- Care coordination
- Capacity optimization
- Payment estimates and processing
- SRemote patient monitoring
- Demand Management
This list often catches healthcare providers by surprise. Any telehealth solution that is not holistic, any telehealth strategy that does not take each of these into consideration is going to increase patient and (especially) provider frustration.
WHY HOLISTIC TELEHEALTH
View Oakkar's webinar for an overview of holistic telehealth -
See The webinar for Telehealth of Tomorrow, today.
Benefits for patients
![]() Increased patient choice
Increased patient choice
- Patients can choose the channel most convenient (or private) for them
- Patients can choose the time of day most convenient (or private) for them
- Patients can choose to switch channels and times without sacrificing their service quality
![]() Faster access
Faster access
- It is often easier for patients and providers to work a telehealth consults into their schedule sooner than in person
- Self-service and automated options allow patients to initiate immediately
![]() Avoid hassles of travel in elderly or child care situations
Avoid hassles of travel in elderly or child care situations
- Travel provides significant barriers for caretakers, especially for geriatric and mental health populations
- Lack of transportation also is a barrier to those who are economically disadvantaged. A 2020 study published in the American Journal of Public Health found Hispanic people, those living below the poverty threshold, and Medicaid recipients were more likely to delay care due to transportation.
![]() Reduced total cost of visit (copay, travel, time off work, etc.)
Reduced total cost of visit (copay, travel, time off work, etc.)
- Copays are often less, and for many during COVID are waived
- According to 2015 research in the American Journal of Managed Care, the average in-person visit takes 121 minutes out of a patient’s day, even though less than 20 of those minutes were with a provider.
- According to a 2019 research brief by Altarum, the travel and wait times for healthcare are longer than they are for government services, like licensing, legal, and insurance!
- The opportunity costs of travel, waiting, and taking time off work are significantly reduced with telehealth.
![]() Better Outcomes
Better Outcomes
- Not surprisingly, in cases where telehealth improves access, it also improves outcomes, as reported by the Agency for Healthcare Research and Quality
Benefits for providers
 Maximize revenue (fill schedule, reduce no-shows, etc.) (without telehealth, you’re leaving money on the table)
Maximize revenue (fill schedule, reduce no-shows, etc.) (without telehealth, you’re leaving money on the table)
- Ease of access means fewer cancellations
- Retain revenue even when staff can’t come to the office
- Self-service scheduling and automation can quickly fill cancelations and appointment gaps
![]() Flexibility with schedules
Flexibility with schedules
- Providers can still conduct telemedicine visits when not in the office
- Staff can perform telehealth-enabled services when not in the office
- Patient schedule changes don’t need to equate to lost revenue, with automated waitlists and rescheduling
![]() Break down silos – improve continuity of care
Break down silos – improve continuity of care
- Most healthcare services today are uncoordinated, and often frustrating
- Investing in holistic telehealth system involves breaking down the barriers and silos in healthcare
- A mature, optimized telehealth system can support over 20 services across roles and departments
![]() Adapt to outbreaks, severe weather events, and the unexpected
Adapt to outbreaks, severe weather events, and the unexpected
- A mature telehealth provider is able to adapt and switch channels as needed without interruption
- This gives your organization more options when the unexpected happens to individuals (e.g. transportation issues), localized events (e.g. power outage), or outbreaks (e.g. pandemic)
- To find out more, see the Patient Service maturity model.
The end result is to become an agile, learning organization that can quickly adapt service models to new situations. A mix of in-person services and digital services are all orchestrated by digital planning and communication. For example - 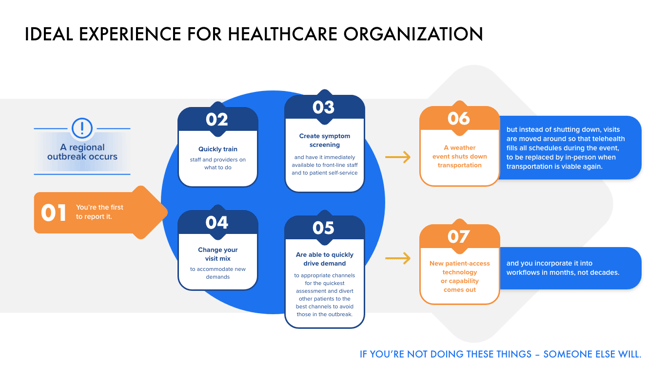
![]() Remain competitive
Remain competitive
- Modern healthcare providers need to adapt
- Many patients want to stick with a provider with whom they’ve developed a relationship
- BUT… about 50% are willing to switch to any provider who is more convenient, a trend that is growing
- See: http://go.sage-growth.com/covid-19-market-report, and https://www.doctor.com/resources/telemedicine
- Direct to patient competition from payers and employers is increasing
- Teledoc and other telemedicine-in-a-box services get patients to bypass local practices and often don’t have allegiance to a particular hospital system
- Telemedicine-in-a-box services have grown considerably
- Competition is soon coming from retailers
- Consider this: for a single item return, Amazon coordinates with shipping, warehouse, suppliers, merchant services, and more without any further customer input. They are used to handling complexity on behalf of customers, earning greater loyalty and allegiance.
- The typical healthcare practice, on the other hand, typically requires the patient to reach out to each party themselves, often playing phone tag with schedulers, nurses, and constantly repeating themselves. This not only results in lower satisfaction and loyalty, but leads to mistakes
- Amazon and Wal-Mart, two of the largest retailers in the world, have started experiments with healthcare delivery with the stated goal of expanding these.
DELIVERING A TELEHEALTH SERVICE WITH QUALITY
– KEONA 6 FACTOR FRAMEWORK
Offering telehealth with the same care and professionalism as in-office services is challenging. However, if you are looking for help in creating a checklist or designing your telehealth delivery, Keona Health is developing the 6-Factor Framework to make it easier for you:
- Service-channel combination
- Finance (costs & reimbursement)
- People (job descriptions & training)
- Tools (technology for delivery, support, and access)
- Safety & Liability (staying compliant)
- Metrics (KPIs for delivery)
Keona 6 factor coming soon
Patient Service MATURITY MODEL
The adoption of telehealth is critical for the future of the healthcare industry. To reap the benefits, however, the entire organization must develop operations and capabilities focused on successful delivery.
It is impossible to go from no telehealth to being a fully mature organization. Standards must be centralized and service silos have to be removed. Technology must be investigated, adopted, and integrated. Learn more about the steps involved here: Patient Service maturity model Take an assessment to understand where your organization’s maturity lies here:
TELEHEALTH CHANNELS, TYPES OF CONSULT, AND REIMBURSEMENT
HRSA defines telehealth technologies as:
“Technologies include videoconferencing, the internet, store and-forward imaging, streaming media, and landline and wireless communications.”
CMS determines reimbursement by channel-service pairs. In other words, the type of consultation, combined with the channel being used, as a pair dictates the type of reimbursement the provider can get (if any). A key step in pursuing a holistic telehealth strategy is to determine which reimbursable services your organization will provide over which channels.
Synchronous communication technology
.png?width=50&name=telemedicine-2%20(2).png) Video Visit - Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, Whatsapp video chat, Zoom, or Skype.
Video Visit - Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, Whatsapp video chat, Zoom, or Skype.
- Services currently reimbursed over video visit: Virtual check-in with (E&M) an established patient (G2012), determining if office visit is needed Providers can be reimbursed for telehealth instead of POS codes at the same rate as in-person. Digital evaluations (99421-99423)
- Many of these options are not fully HIPAA compliant. During the COVID crisis, there is a special waiver (see Safety and Quality below). The problem is that this is only temporary, leaving providers who use Facebook, Google Hangouts, Skype, and regular Zoom in danger of steep penalties.
.png?width=50&name=telephone-1%20(4).png) Telephone (including video visit with low bandwidth) – landline, wireless, or internet real-time voice options.
Telephone (including video visit with low bandwidth) – landline, wireless, or internet real-time voice options.
- During COVID, some audio-only visits are reimbursed at the same rate as in-person visits. It is useful for providers to know what audio visits are reimbursable, even at reduced rates, in case technical difficulties, such as low bandwidth, keep the video portion of the video visit from working properly.
- Voice-only reimbursement: These are virtual check-in (E&M) - the patient must initiate, they must consent verbally to receive virtual check-in services, and the communications must be within a 7-day period.
.png?width=50&name=chat-1%20(2).png) Web chat - Signal, Jabber, Facebook Messenger, Google Hangouts, Whatsapp, or 5 iMessage. Typically, these platforms employ end-to-end encryption, which allows only an individual and the person with whom the individual is communicating to see what is transmitted.
Web chat - Signal, Jabber, Facebook Messenger, Google Hangouts, Whatsapp, or 5 iMessage. Typically, these platforms employ end-to-end encryption, which allows only an individual and the person with whom the individual is communicating to see what is transmitted.
- Web chat is unique in allowing real-time private discussions with people who are otherwise within earshot of others. Video visits and even audio conversations can lack privacy.
- Reimbursement: web chat is not approved as a distinct channel by CMS. It is viable for reimbursement for the same items as store-and-forward communication (see below).
See all CMS synchronous telehealth reimbursement codes, including which are available for audio-only, here: https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes
Asynchronous messaging technology
Online messaging (“store-and-forward”) – asynchronous messaging can remove wait times, and overcome language and cultural barriers. It has been especially effective for specialties like dermatology or even urology where imaging is important. Advanced providers are using real-time chat, asynchronous texting, online messaging facilitated by web AI.
.png?width=50&name=live-2%20(3).png) Store-and-forward includes streaming video messages, like MarcoPolo.me.
Store-and-forward includes streaming video messages, like MarcoPolo.me.
- Only a few services are currently reimbursed over store-and-forward: medicare part B has 3 codes for e-visits. Relegated to established patients, patients must initiate, consent to the evisit, and communications must be within a 7-day window. Medicaid is very limited for store-and-forward, with only 15 states reimbursing.
.png?width=50&name=email-1%20(2).png) SMS messages & email
SMS messages & email
- Must be secure, or you will run afoul of HIPAA guidelines. See Safety and Quality below for more.
- Limited reimbursement as eConsult under Medicare codes 99451 and 99452
.png?width=50&name=fax-1%20(2).png) Fax
Fax
- Believe it or not, fax is still a major communication medium in healthcare!
As a patient channel, however, there is no reimbursement
For more information on reimbursement
Please refer to:- CMS Official list of telehealth codes: https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes
- MGMA COVID Coding Cheatsheet: https://www.mgma.com/resources/revenue-cycle/covid-19-coding-cheatsheet (MGMA membership required)
KEY TECHNOLOGY CAPABILITIES FOR TELEHEALTH SECURITY
HIPAA Compliance
The Health Insurance Portability and Accountability Act (HIPAA) defines rules around privacy. Together with HITECH, they define data that must be protected within a healthcare context.
Protected Health Information (PHI) – health information that can be linked to an individual must be protected. This means that only authorized users should have access to PHI.
- Transmission – all communication, including data “in transit” over the internet, but be secured
- Data storage – all data containing PHI, including recordings and consult notes, must be secured
- Monitoring – a system of monitoring must be in place to identify accidental or malicious breaches should they occur
- Business Associate Agreement – Software and vendors that perform services and store data on behalf of the provider need to sign a business associate agreement. This is a partnership agreement stating that the business associate will assume legal liability for protecting the PHI in accordance with HIPAA guidelines.
Be sure all your technology partners can support the HIPAA guidelines and that they are willing to assume the legal liability for doing so.
For more information, see: https://www.hipaajournal.com/hipaa-guidelines-on-telemedicine/
HIPAA Waivers during COVID pandemic
In March of 2020, the Office for Civil Rights announced that they will not enforce violations of HIPAA for good-faith efforts to delivery telehealth during the COVID-19 crisis. This was expanded in April. During this time, many providers are using technology, such as Zoom and Skype, without signing a business agreement or following HIPAA guidelines.
These measures, however, are only temporary and long-term solutions will have to meet all HIPAA guidelines.
Sources:
Find all published bulletins here: https://www.hhs.gov/hipaa/for-professionals/special-topics/hipaa-covid19/index.html
For another summary, see: https://www.hipaajournal.com/hipaa-compliance-and-covid-19-coronavirus/
SAFETY & QUALITY
Telehealth safety includes software and staff. In order for telehealth to be delivered with safety and quality, HIPAA Compliant Telehealth Software must be used and integrated into every step of the workflow. Also, whenever any healthcare staff member encounters a situation that might be unsafe, they need to quickly identify it and take appropriate steps to address it.
- Safety tools – Identifying a situation as unsafe can itself be tricky. Everyone may know that chest pain or severe loss of blood may indicate life threatening risks, but many symptoms that are just as threatening are more subtle or less known. The telehealth software should provide tools to help ensure patient safety. These can vary from simple safety checklists (often called “red-flag” lists) incorporated into the software, to sophisticated NLP Symptom Algorithms. These should identify the level of risk and also the next steps to take to appropriately address that risk. The level of risk is usually classified on a time-scale of when the patient should be evaluated by a qualified professional. If nurses are part of the safety and escalation process, it helps if Nurse Triage functionality is included. These tools help a nurse perform clinic triage services, give care advice to patients, and document the results.
- Escalation process tools – After identifying a potentially unsafe situation, the next step is getting the patient evaluated by a qualified professional. This is called escalation, and each provider organization sets up its own processes and procedures for escalation. These may change based on the location of the patient and the time of the day. The telehealth software should have these escalation procedures built in: if the next step is to have the patient talk to a nurse, staff should be able to make that happen with just a click. If the next step is to page a provider, the software should be integrated with the paging software and know the on-call schedule, to facilitate one-click or even automated paging.
- Geolocation & e911 – There are some cases where internal escalation is not the answer. The patient needs 911 right now! While staff can tell the patient to call 911, this introduces delays and risks if the patient doesn’t agree, isn’t in a position to do so, or isn’t able to explain their situation properly. Best practice is for your staff to get the correct 911 on the line themselves. For these situations, software that integrates with geolocation capabilities tied to e911 services can get the correct 911 service on the phone with the patient without delays.
INTEGRATIONS WITH YOUR EXISTING TECHNOLOGY

- White-label website integration – Any 3rd party telehealth tools accessible directly by patients should be white-labeled. This means they carry your brands, use your colors, and look like your site.
First of all, when patients go to your website, they should see the telehealth tools easily available.
Second, access should be easy. If the patients can access basic telehealth services without passwords and account maintenance, even better! Third, the best telehealth tools facilitate patient self-service for reducing costs and improving patient satisfaction. They can be tailored to fit your workflows to reduce work and optimize quality
- Practice Management (PM) integration– Without PM integration, telehealth runs the risk of being another siloed application. Telehealth workflows should be smoothly incorporated into the rest of the organization’s workflows. With the right type of scheduling tools built-in, you can get added benefits of automating visit and provider requirements and even opening the entire schedule up to self-scheduling
- Electronic Health Record (EHR) integration – Integration with the EHR brings a lot of benefits. First, the integration should display the patient’s health context into the telehealth software to facilitate proper decision making. The documentation and results of all telehealth services should be written back to the patient’s chart so the EHR continues to be the source of truth for the patient’s health record.
- Computer-Telephony integration (CTI) – While video chat gets the most reimbursement, audio-only telehealth still gets the most volume. CTI enable a single system for all your telehealth needs. This allows unified documentation, less staff training, and even the ability to swap between contact channels smoothly. CTI also brings lower handle time.
- Sales / Marketing (S&M) CRM integration – Once you have sophisticated telehealth abilities, let the world know! Incorporate self-service links into your campaigns, or convert market leads directly into patients quickly with S&M CRM integration.
WHAT ARE THE COSTS OF TELEHEALTH?
.png?width=50&name=telemedicine-2%20(2).png) Reimbursement: See Telehealth Channels above for an overview of reimbursement.
Reimbursement: See Telehealth Channels above for an overview of reimbursement.

![]() Expense: According to MGMA (“Performance and Practices of Successful Medical Groups” accessed 10/13/2020), within most medical groups, there are 3-8 full-time employee’s (FTE) for every physician. According to statista.com (accessed 10/13/2020), there are 16 FTE’s for every physician in US hospitals. These roles support the process of providing healthcare in a number of ways – from scheduling, to computer maintenance, to billing, to nursing, and more. Many of these resources must be “provisioned” to support providing medical service – in other words, when a healthcare service is scheduled, some of their time needs to be dedicated to help deliver the service.
Expense: According to MGMA (“Performance and Practices of Successful Medical Groups” accessed 10/13/2020), within most medical groups, there are 3-8 full-time employee’s (FTE) for every physician. According to statista.com (accessed 10/13/2020), there are 16 FTE’s for every physician in US hospitals. These roles support the process of providing healthcare in a number of ways – from scheduling, to computer maintenance, to billing, to nursing, and more. Many of these resources must be “provisioned” to support providing medical service – in other words, when a healthcare service is scheduled, some of their time needs to be dedicated to help deliver the service.
Reducing telehealth costs is a far-reaching subject. But given the enormous expense of support staff, the biggest cost-savings can be found through pursuing just two concepts:
- Add automation to telehealth processes
Automation reduces the FTE ratio per provider. A Healthcare CRM is a tool that smooths this provisioning with advanced automation and often artificial intelligence. This automation improves service, reduces cost, and maximizes the schedule. For more information see “What is a healthcare CRM?”
- Break Down Silos and Cross Train Employees
Cross training employees has two benefits. First, when telehealth queues get overrun, more resources are available to help out due to cross training. Second, a well-implemented cross-training program means that functions don’t have to calculate expense growth and reduction at full FTE, but partial employee time can be devoted to other functions, further reducing costs.
For more information on breaking down silos, see our Patient Service Maturity Model.
MANAGING TELEHEALTH WORKERS
Hiring for Telehealth
Job descriptions need to change when you are hiring for telehealth as it is different from in-person in many ways.
- First, there are the demands; telehealth workers consistently report higher stress than their in-person counterparts. Part of this is simply that efficient telehealth has a higher volume, and the other part is that each interaction is unexpected. A telehealth worker could be telling someone to call 911, followed by a normal visit, and then a chaotic scenario like suicide or stroke. Therefore, you should look for someone who is empathetic but doesn’t get easily flustered and stressed.
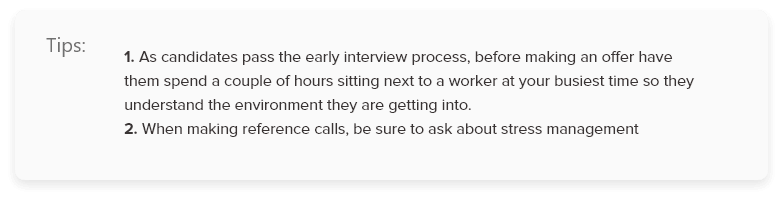
-
Second, listening needs to be more active, because signals are easier to miss in telehealth situations. It’s also easier for the patient to misunderstand what you are saying. Therefore, make sure that at least one of your interviews is remote to get a sense for how they communicate over the phone and video. Do they know how to maintain control of the call while also slowing down and making sure they are hearing and being heard? For more information on telehealth communication, read “The Importance of Active Listening” by Gina Tabone.
- Third, telehealth requires more technology interaction. You want to assess how they navigate technical issues; typing tests also tend to be more important.
For more tips on hiring, check out this Practical Dynamite episode:
Training for telehealth
Hiring the right staff is just the beginning. Training for telehealth includes all the elements you typically train for – job duties, company policy, technologies – and then adds these additional topics:
- Navigating telehealth technical issues
- Communication skills
Communication failures are a real problem in telehealth. All telehealth staff should be trained in to develop their tele-presence and telephony-side manners.
Practical Dynamite Episodes and Downloadable Resources:
 Active Listening Podcast + 8 Tips
Active Listening Podcast + 8 Tips
 Telemedicine Communication with Seniors
Telemedicine Communication with Seniors
- Telehealth safety
All roles delivering healthcare service, including nonclinical roles, need to be trained in identifying potential issues, escalating care, and navigating emergency process.
- Remote emergency situations
Helping patients in emergency situations usually comes down to geolocation and e911 for patients. Every employee engaged in telehealth should be trained and practice in handling emergency situations
Managing for telehealth
- Managing remote workers
- Preventing burnout
Telehealth jobs are known for higher burnout. This is due to a combination of fast-paced, unanticipated situations, and the complexity of telehealth workflows and tools. A telehealth worker could be telling someone to call 911, followed by a normal visit, and then a chaotic scenario like suicide or stroke.
Posted By

Stephen Dean is COO of Keona Health, where he’s spent 13 years building AI systems that transform patient access. Before “agentic AI” was a term, his team was deploying autonomous systems that now handle millions of patient conversations annually.
Related Post
November 19, 2024
heading into 2025, healthcare organizations face increasing pressure to digitize...
October 18, 2023
is your healthcare call center getting crushed under the weight of frustrated...





