“Telehealth is here to stay.” – Learn how to optimize its use for better outcomes
Telehealth and long-distance clinical healthcare (online healthcare) is essential in the modern telemedicine environment.
Most providers have been building their telehealth vehicle while driving down the COVID highway; they haven’t had a blueprint for consumerism and the digital front door. Their telehealth practice is still not up to speed.
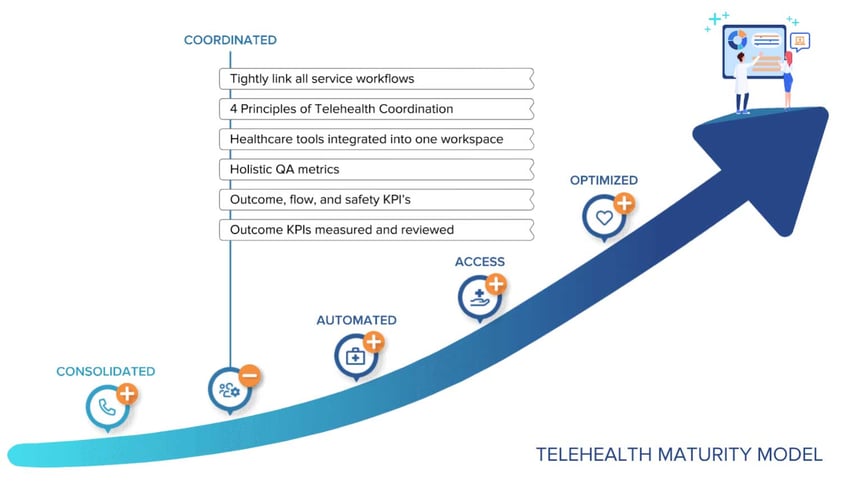
The truth is, exceptional patient experiences only come from beautiful team experiences. The realities of complex healthcare service is that you cannot focus on the patient unless you've first focused on your team. This model identifies the path your digital transformation must take for your team to deliver on an amazing digital front door. Keona’s Patient Service Maturity Model will help you accelerate from zero to 100.
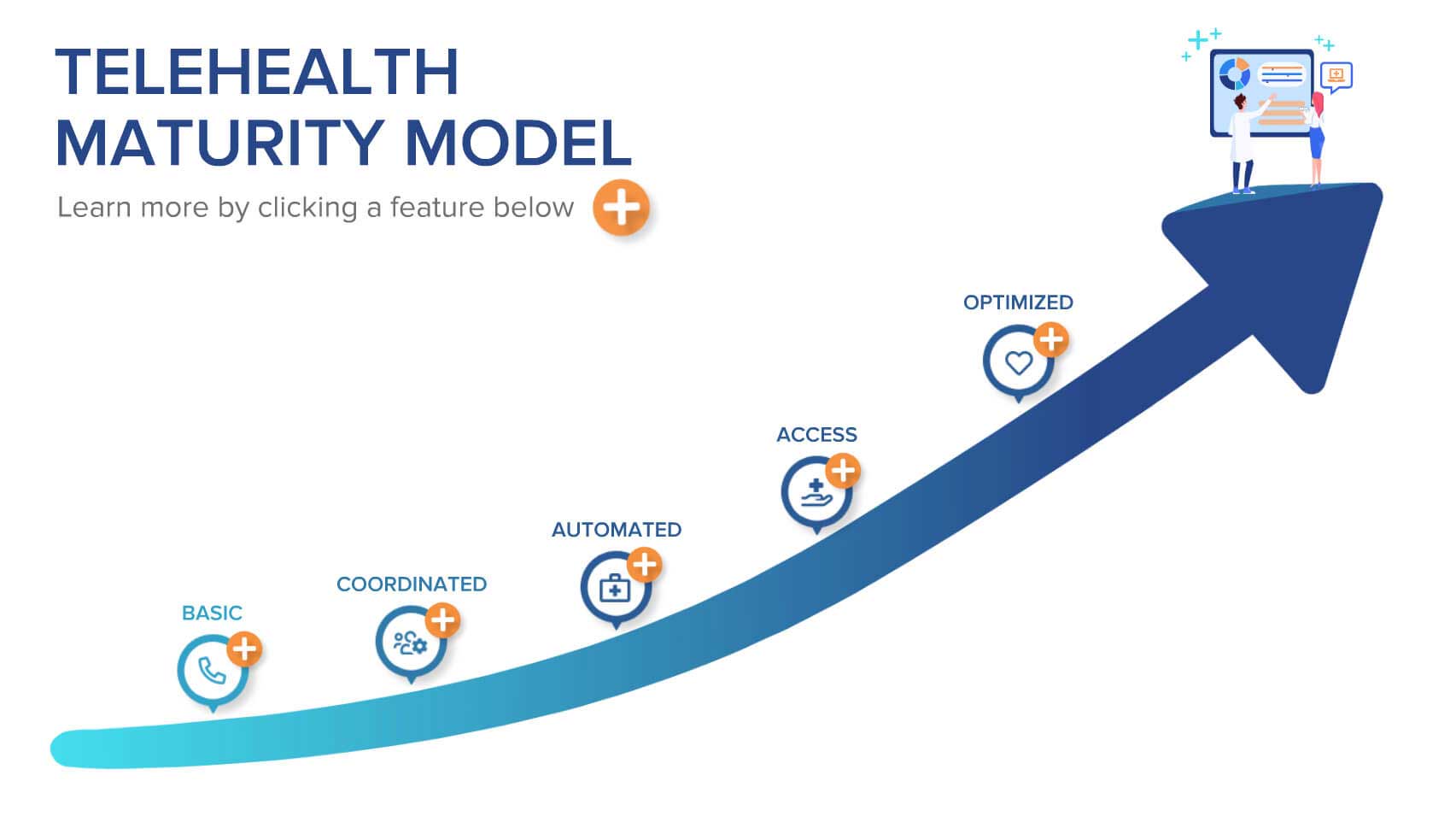
WHAT IS A MATURITY MODEL
A maturity model is a roadmap to excellence. It shows the path that must be taken to adopt any new telehealth need & outlines the core competencies for continuous improvement.
Like any skill an entire organization must develop, exceptional delivery in telehealth is like eating an elephant: it is easy to quickly feel overwhelmed. One of the key purposes of a maturity model is to help break the giant down into “bite-sized” pieces.
Ultimately, however, it is a process improvement tool. If you’re interested in other maturity models in healthcare, check out these other models
Executive Summary
The Patient Service Maturity Model is about your organization’s core capabilities & adaptability.
-
CONSOLIDATED
Your organization has determined that telehealth is a strategic priority. Consolidation is the process of bringing all support processes together under unified leadership and a consistent toolset, including a Healthcare CRM.
Why: Telehealth needs to be a strategic goal from the top of your organization including investing in the tools to support it. If the consolidation step is skipped, the barriers to coordination will still be in place and the telehealth change project will fail or take a VERY long time.
-
COORDINATED
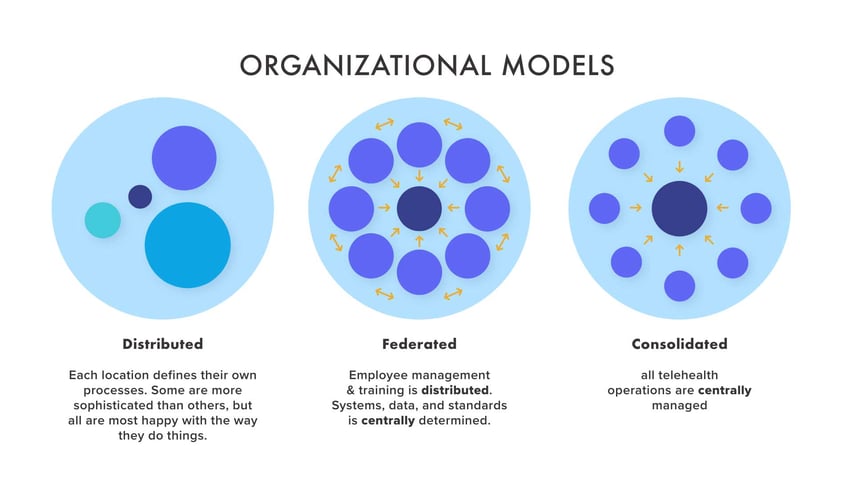
Coordination is the process of manually linking all the workflows together and training a small team on performing them end-to-end. You are able to take into account the full patient context & service is delivered with continuity. Team members are cross-trained in other functions. Service delivery is federated or centralized. See below.
Why: Breaking down barriers between silos in data, roles, & medical specialty is critical to holistic telehealth. This structure of coordination is what makes it possible to deliver on the 4 principles of telehealth delivery. The manual work of mapping out and documenting the workflows is the most difficult for many healthcare organizations, but also the most important. Until you have figured out how to coordinate & consolidate workflows, you will be automating the wrong things.
-
AUTOMATED
Automation takes the coordinated workflows and makes them more efficient, consistent, and safe. The improved, coordinated workflows defined in step 2 are simplified within a unified workspace. Training time is reduced, quality and interaction time are improved, as are documentation and tracking. Management is simplified across all channels.
Why: If Automated is skipped straight for patient access, patients will be given online tools, but they will be frustrating and clunky. The patient won't feel like they have the same support they get when they call in.
-
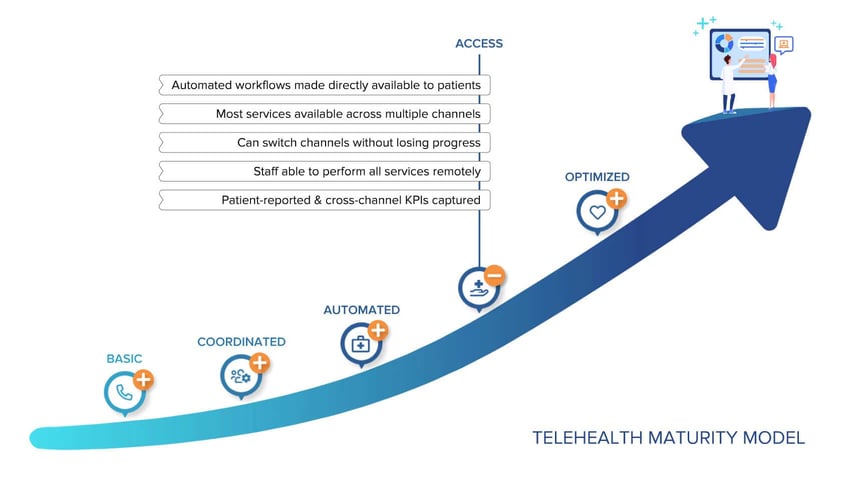
ACCESS
The above automation is made available directly to patients. Service delivery is agnostic, so patients & staff move between channels with minimal disruption.
Why: Patient satisfaction goes way up when you give patients the flexibility & control of self-service. Costs drop as patients handle tasks themselves that your staff used to perform. Developing multiple channels are key to increasing patient access & organizational flexibility.
-
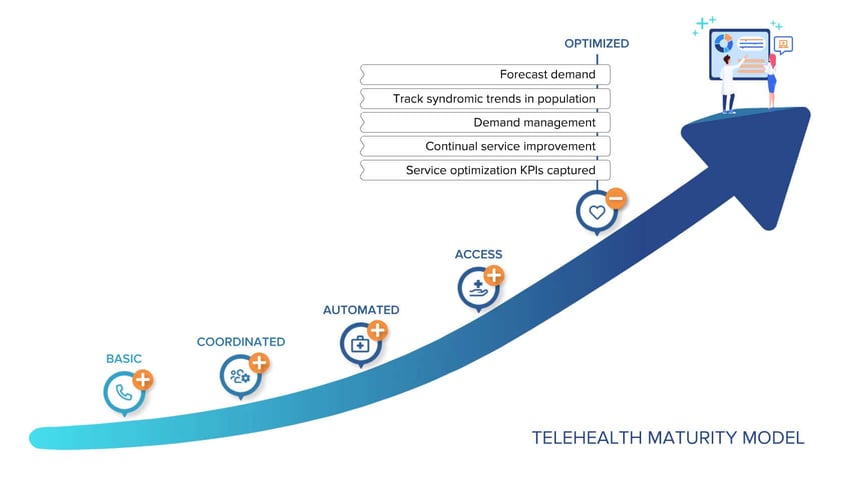
OPTIMIZED
The organization is ready for continuous service improvement to any patient trend. Staff cross-training is deep, allowing maximum flexibility. The organization can shape demand management & even confidently offer satisfaction guarantees.
Why: Rapid analysis, response & implementation make practices more flexible, more adaptable & more streamlined. It is the key to confidently facing changing circumstances.
The organization is now ready for continuous service improvement to any patient trend. Staff cross-training is deep, allowing maximum flexibility. The organization can shape demand management & even confidently offer satisfaction guarantees.
If you are responsible for implementing a single service, like telemedicine or scheduling, but don’t have the ability to change your organization’s mission & strategic direction, check out Keona's 6-Factor Framework (upcoming)
THIS MODEL IS FOR ALL TELEHEALTH
When most people think of telehealth, they think only of a provider visit over video chat. Telehealth as defined by the US Dept of Health & Human Services is your entire digital front door.
The federal agency defines telehealth as using any remote technology to support long-distance clinical health care. Not just real-time video, this includes telephone, web chat, as well as over asynchronous SMS texting or secure messaging. Even digital scheduling and check-in are part of telehealth. It includes sending pictures along with online applications such as patient portals. What is more, this definition of telehealth includes not only the remote delivery of healthcare, but also preparation & administration of remote healthcare.
To see how broad & deep telehealth can be, follow this diagram. It shows the services that are typically rendered around a single telemedicine visit. A smooth telemedicine visit relies on sophisticated coordination across many services including administration & health education.
For more information on the scope of telehealth, see the The Ultimate Guide
What are the Benefits of a MATURE Telehealth Workflow?
You have probably experienced the benefits of digital transformation as a consumer. When you contact Amazon, your airlines, or even Roto-Rooter, they recognize who you are by the number you are dialing from. The person taking your call has at their fingertips your entire purchase history, your preferences, & instructions on how to handle nearly every request or complaint you make. If, for some reason, they are unable to handle your call & have to forward you to someone else, you can be sure that your notes are available for that next person. The new person may verify key pieces of information, but you can be confident you won’t have to repeat every single word that you said.
When you call your healthcare provider, you face very different experience.
It doesn’t have to be this way. Mature telehealth providers can offer the same advantages of consumerism as what you experience elsewhere.
What are the Patients' Benefits?
- Increased Choice
- Faster Access
- Reduced total cost of the visit
- Easier Care - especially for elderly and children
- Better outcomes
What are the Organizational Benefits of Telehealth?

- Increased Revenue
- Flexibility with schedules
- Improved continuity of care
- Adapting to the unexpected
- Remaining competitive
This is just the beginning.
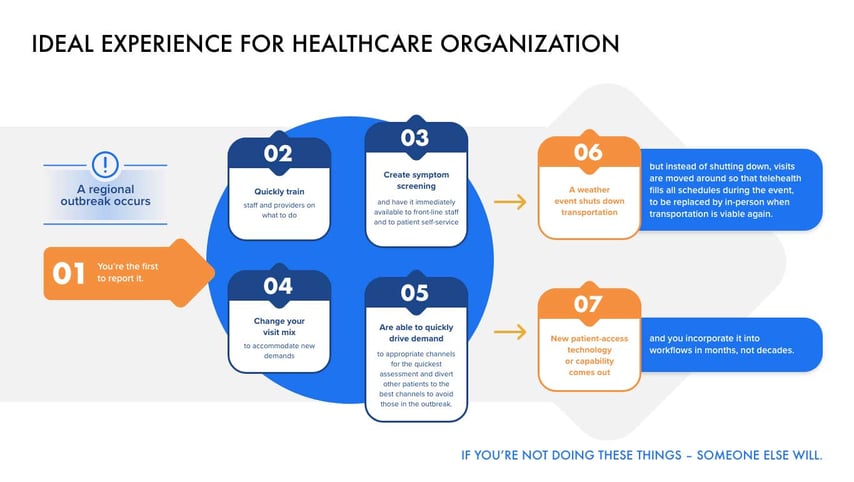
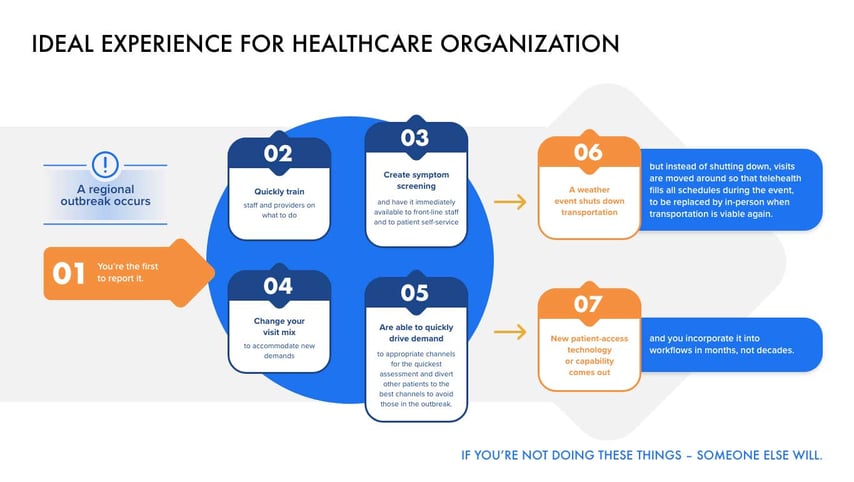
Once an organization reaches telehealth maturity, they are less susceptible to the shocks of unexpected events. This is because the core competencies of managing telehealth workflows make them nimble & adaptable. They are aware of the syndromic trends in their population without looking at the news stand. They can quickly create new health assessments & resulting workflows & make them available to their staff & online. They can create new visit types & customize them for each provider. They can direct patient demand to the most optimal channels for the moment.
Examples of the adaptability of the mature telehealth organization:
To see more details about the benefits of telehealth, please refer to The Ultimate Guide
Telehealth MATURITY IN DETAIL
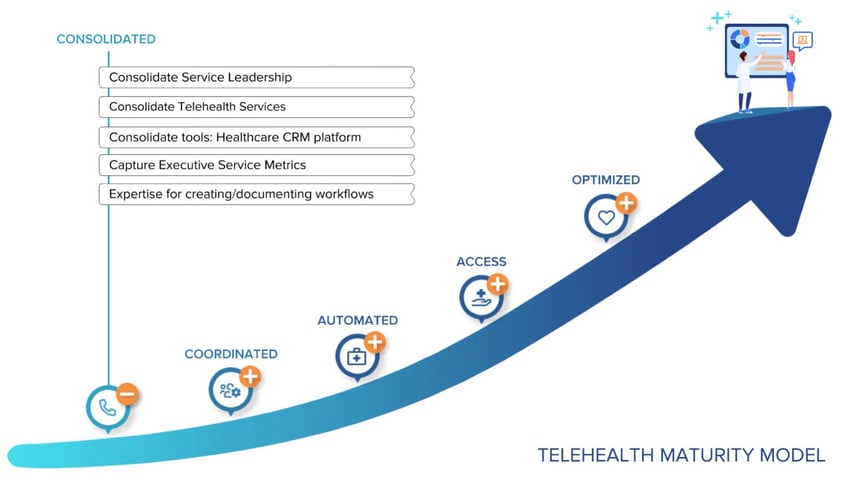
CONSOLIDATED
Summary
Consolidation is the process of bringing all support processes together under unified leadership and a consistent toolset. Before consolidation, the different steps needed to help a patient are performed by different people scattered across different departments. The barriers of too much specialization, different departmental agendas, and just distance and unfamiliarity must be overcome. If the consolidation step is skipped, the barriers to coordination will still be in place and the telehealth change project will fail or take a VERY long time.
Practical Steps
- Unify service leadership
- Consolidate at least 3 or more telehealth services onto a workflow platform
- Have expertise for documenting workflows & creating new training programs
- Healthcare CRM
- Capture executive metrics & call reaction metrics
In Depth
| Unify service leadership. |
Why centralized service management is necessary:
- Your workflows cannot be truly coordinated if they are different for everyone
- You can have variations to meet requirements for each specialty, location, & provider, but you must have a shared core set of data, systems, & standards to implement automation.
Steps you should take:
1. Setup a cross-department taskforce for unifying telehealth services & workflows
2. Identify measurable goals
3. Determine if you will centralize (pro’s & con’s)
- Faster to train
- Easier to implement
- Harder to keep providers & patients happy
- The key is for the software to incorporate the differing requirements of each location & provider.
OR
4. If you will federate (pro’s & con’s)
- Longer to roll-out
- Longer to train
- Easier to keep each practice & provider happy
- As with centralized, the key is for the software to enforce location & provider requirements in scheduling & workflows.
| Capture executive service metrics |
Why capturing executive service metrics is useful
- Executive service metrics are holistic measures of your organization's service. Patients may rate each interaction very highly, but be very disappointed with your overall service. These metrics focus on the big picture.
- Establishing the baseline for these metrics now will help you measure progress as you work your organization through the maturity model.
1. Define service mission & goals
2. Define markets & services for focus
3. Create cross-functional leadership team to advocate & review following metrics
- Net Promoter Score
- Customer Ease Score
- Customer Satisfaction Score
- Revenue Growth
- Patient churn
| Consolidate telehealth services |

Why consolidating telehealth services is crucial
- Thorough mapping of workflows improves accuracy
- Workflow guides improve team consistency
- Training length is reduced when the software itself guides users through the workflow
Steps you should take
- Determine the metrics to track based on executive Mission & Goals
- Determine the channels initials services will be delivered over
- Map out all the related services that come before & after (basic workflow mapping)
| Consolidate tools: Healthcare CRM Platform |
Why Implementing a Healthcare CRM is crucial
- CRM manages interactions across time for users and facilitates patient level data analysis
- Consolidating onto a single platform reduces mistakes and mental burden of users
- Workflow tool should contain healthcare specific safety tools
- Healthcare government mandated privacy and security standards, including breach identification & handling
Steps you should take
- Read more about Healthcare CRMs on Wikipedia
- Understand the basics of a Healthcare CRM
- Ensure the technology you choose meets HIPAA & security guidelines
- Choose more than a technology - choose a solutions partner who understands healthcare transformation
- Choose a vendor who can offer you the same level of service that consumer services require
(Related: Understand the difference between a sales & marketing CRM and a healthcare CRM)
Few healthcare technology companies have optimized their own workflows for consumer-level service & support.
COORDINATED
Summary
Coordination is the process of tightly linking all the workflows together and training a small team on performing them end-to-end – basic scheduling, complicated scheduling, nurse triage, payments, case management, etc. Before coordination, it is up to the patient to follow-up and be sure all the dots are connected. If the coordinated step is skipped, your programmers and tools will be automating bad workflows.
Practical Steps
- Follow the 4 Principles of Telehealth Coordination
- Tightly link all service workflows
- Workflows are documented, accessible to everyone across silos, & staff are cross trained
- Healthcare tools are integrated into one workspace
- Extended team members are trained in telehealth safety, documentation, & soft skills
- Holistic QA metrics are in place and reviewed for all telehealth roles
- Outcome, flow, and safety KPI’s are part of service metrics
In Depth
| Follow the 4 Principles of Telehealth Coordination |
The key to all of this is to transform your team's experience so it is smooth and easy to support patients. This means coordinating between the silos that exist between providers, departments, as well as care staff, and even between sites & specialties. Key tools, such as medical records & pharmacy data should be integrated.
While there are a lot of tasks, the 4 key principles behind great service are rather simple:
- Every decision point has full patient context
- Each step in the workflow is aware of steps before & after
- Provide all the services in one interaction – while the patient on the phone, online, in person
Ideally, no transfers or callbacks.
- Services are connected across every channel
| Tightly link all service workflows |
Why coordinated workflows are crucial:
- Patient satisfaction depends on quick resolution, minimal transfers, with minimal patient effort.
- You cannot automate workflows without first coordinating service efforts
If you automate without this step, you lock yourself into disjointed and painful workflows
- This step prepares staff for future agility - they'll be able to quickly handle any change.
Disjointed vs Coordinated workflows
- Today’s healthcare workflows are incredibly disjointed. Take the scenario of someone who schedules a visit, but has symptoms that need to be triaged. During the visit the provider refers the patient to a specialist:
TELEHEALTH TODAY
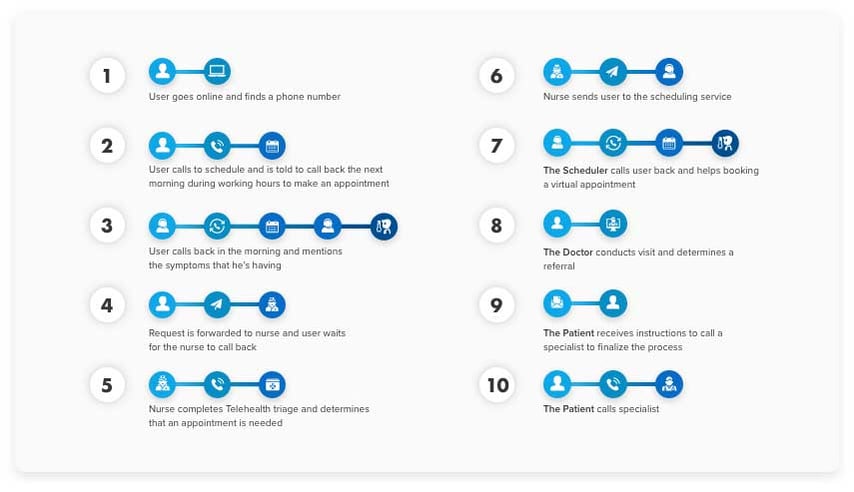
This example is all to common. It violates all four of the key principles:
- Every decision point has full patient context: Each person the patient talks to only has partial information
- Each step in the process is aware of steps before & after: Those handling any one step in this workflow are unaware of next steps
- Provide all the services in one interaction: Each service is provided in a separate interaction.
- Services are connected across every channel: changing channels means the patient must repeat information given before. In other words, the data is “lost” when switching channels
This large number of steps is due to the care not being coordinated. Harvard professor & management thought leader Clayton Christensen noted in his book “The Innovator’s Prescription,” that healthcare works in batch processing. Services are provided by independent groups that “dump” work to the next group where queues build up behind each one. Every person is trained in just their own tasks and unaware of what others are doing.

COORDINATED TELEHEALTH
Coordinated workflows are designed to take into account the four key principles. The exact same scenario, when following the 4 principles, only takes 4 steps:
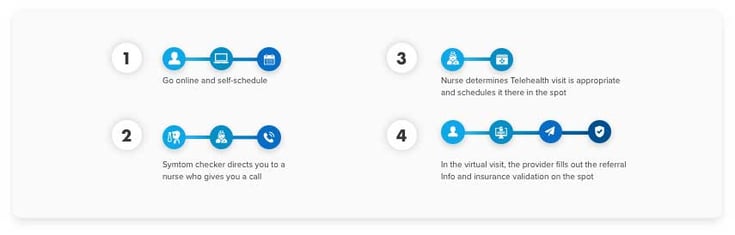
The 4 principles are key to coordinated care. Information is not lost & each person's work is closely coordinated with everyone else's work.

Steps you should take:
- Map out your workflows
- Find ways to consolidate stages as much as possible
- Build the workflows into a workflow tool, like a Healthcare CRM, accessible to all
- Implement a single Healthcare CRM that brings all the patient’s data together from all of your systems as much as possible. These should include:
- PM
- EHR
- Telephone (CTI)
- Knowledge Base
- Clinical Decision Support
- Messaging
- Sales/Marketing CRM
- Geo-location Services
- Patient Monitoring
Real-life Example 1: telephone patient intake immediately following scheduling
With the advent of COVID, providers were having a tough time in the video visits due to the lack of an intake process & pre-visit summary. Some clients have switched to complete the intake process at the time of scheduling. Not only has this change smoothed out their virtual visits, it also has smoothed out office visits as well. There are fewer people in the waiting room & fewer delays throughout the day. This is an example of principle #2 (“each step is aware of steps before & after”) & principle #3 (“provide all the services you can in one interaction – while the patient is online / on the phone”), because the person scheduling the visit is told what the intake process needs to look like for each type of visit & they perform as much as they can on the spot.
>Real-life Example 2: everyone is trained in scheduling
We work with clients to train all staff who interact directly with remote patients how to schedule. Using automation like Intelligent Scheduling makes this possible. Nurses, medical assistants, & even technicians can quickly schedule while talking with a patient. If they don't have time? Just quickly send the patient a link to schedule themselves in real-time! This minimizes patient leakage, saves the patient’s time, avoids transferring the patient, all resulting in higher patient satisfaction & a fuller schedule.
This is another example of principle #3 (“provide all the services you can in one interaction”).
| All staff are trained in Telehealth safety, documentation, & soft skills |
Why this is crucial:
- Telehealth communication is significantly different than in-person communication
- Telehealth safety considerations are unique for two reasons: first, clinicians don’t have the same feedback they get in person. Second, getting a remote patient to the right location is more difficult than when they are in your office
- Telehealth workers consistently report higher work stress than in-person delivery. Higher levels of support & training are needed
Steps you should take:
- Look to American Telemedicine Association for content for telehealth training
- American Academy of Ambulatory Care Nursing (AAACN) has perhaps the most extensive guidelines & recommendations for telehealth, focused on nursing
- Keona Health blog & Gina Tabone regularly publish tips & checklists for telehealth
| QA metrics exist for all Telehealth services |
Why QA metrics are crucial:
- You need objective measurements of quality as you implement change to guide & correct the changes
- Proper governance is required for optimal outcomes
| Outcomes & Safety Metrics |
Why Outcome and Safety Metrics are crucial:
- You can’t optimize what you don’t measure
- Safety & outcome metrics are necessary to truly understand your service quality
Steps to take:
- Record & report the outcome of the encounter
- Did the encounter end with a triage disposition? What was it?
- Number of escalations, & reasons why
- QA ratings / reports
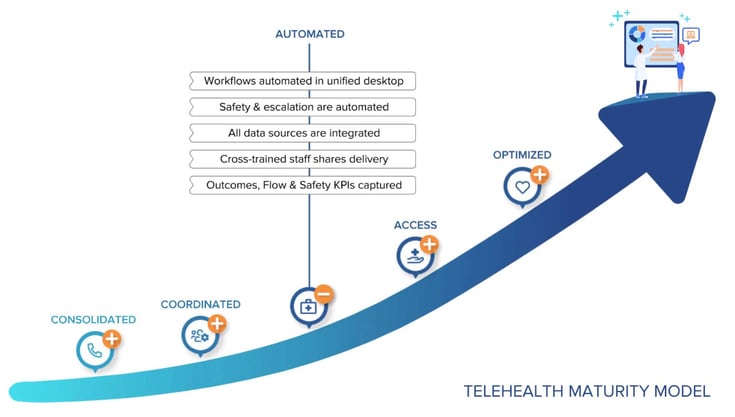
AUTOMATED
Summary
Automation takes the coordinated workflows and makes them more efficient, consistent, and safe. This automation prepares the way for fully digital patient access.
Practical Steps
- Unified desktop automates workflow steps, documentation, safety checks, & escalation procedures
- Patients can access healthcare services over multiple channels
- Proactively intervene & recommend services based on patient context
- Captures Outcomes, Flow & Safety KPIs
- Have results KPIs across each channel
In Depth
| Turn workflows into automation |
Why automation is crucial:
- Automating workflows reduces errors, reduces training time, & reduces costs
- A single interface & toolset across roles facilitates easy administration & allows different roles to assist each other
- It sets the stage for self-service & cross-channel service. Without the simplification of automation, patients could never be trusted to navigate complicated workflows.
Steps to take:
- Subject Matter Experts (SMEs) builds triggers, criteria, & decision points into the software
This is a lot easier once the workflows have been built out in the prior steps. Items to automate or semi-automate include:
- Visit type requirements by specialty
- Provider requirements
- Insurance requirements
- Intake criteria by visit type
- Forms request process
- Customer support process
- Any other telehealth workflows needed
- Encounter routing to staff is built on training & skill sets
One of the key principles is that the workflow is aware of steps before and after the current one. Part of this is understanding the specialized skills of staff so that automated routing and handling can quickly match patients to those who have those skill sets.
- Integrated Knowledge Base for reference information displays based on call type
The best type of knowledge base is the one you don't have to search. You want a system that auto-delivers the relevant knowledge to your users based on the patient, call type, specialty, practice location, or even physician being scheduled.
Learn more about Care Desk Knowledge Base here.
| Prioritize safety and escalation automation |
Why this step is crucial:
- Encapsulating safety checks & escalation procedures improves safety & outcomes
- There are penalties and liability for handling patient inquiries in an unsafe manner
- Online access has historically been lacking safety features and guidance
Steps to take:
1. Incorporate Advanced AI tools & clinical decision tools into the workflow. Key tools:
- Natural Language Symptom algorithms
- Triage Nurse algorithms
- Patient monitoring
2. Establish escalation logic & messaging
- On-call & 2nd level triage logic & integrations
- E911 service integration
- Geolocation & emergency room mapping
- Integrated Fax / EHR messaging to Emergency Departments
- Messaging templates to save precious moments in critical situations
| Captures encounter handling metrics in real time |
Why this step is crucial:
- Call handling metrics give you the tools for identifying issues in call flow & addressing them as they occur
- Gives insight into where automation can improve & also where automation is not helping
- These are also key metrics for staff training & for reducing costs
- This sets the stage for demand management, where demand is forecast & patients are directed to different channels or avenues to facilitate the best service
Steps to take:
- Be sure all your channels (synchronous & asynchronous) report the following metrics:
- Time for each step in the service flow
- Total Handle Time
- Number of interactions per resolution
- Average speed to resolution
- Number of complaints
DIGITAL ACCESS
Summary
Congratulations! If you've reached this stage, you have made it far easier for your teams to assist patients. They are guided each step of the way, and many of their tasks are automated. Now you are ready to throw open the digital front door and bring the benefits of digital transformation directly to consumers.
The key principal for digital access is this:
WHEREVER AND WHENEVER A PATIENT NEEDS ACCESS, THEY OR A CAREGIVER CAN REACH OUT OVER ANY CHANNEL TO FIND REAL-TIME SERVICE.
The Digital Access stage builds on the workflow optimization & automation of the last two phases. It makes services available anywhere over multiple channels with online & AI-optimized cloud technologies.
- Patient self-service is available for most services & workflows, complete with safety checks & escalations
- Patients can switch between channels without losing prior work
- Software facilitates all remote staff workflows .
- Pricing of services is transparent
- Capture patient-reported & cross-channel KPI’s
In Depth
| Patient self-service is available for most services & workflows,complete with safety checks & escalations |
Why Patient self-service is crucial:
- During COVID, clients were overwhelmed with COVID calls. It backed up queues, made clients miss appointment calls, & caused delays in care.
- Self-service offloads work from your staff, freeing up personal queues for those patients & requests that require a more personal touch
- Self-service improves patient satisfaction
- Multiple patient facing channels are required to support the Optimized stage, especially dem& management
Steps to take:
1. Take existing workflows & automation built for your staff & put them on a patient-facing web page.
Key workflows:
- Symptom Algorithms
- Scheduling
- Health education
- Check-in & intake
- Billing & payments
2. Edit the language to be patient-friendly
3. Add pictures, profiles, maps information & other patient-facing content to add ease & instill confidence
| Patients can switch between channels without losing prior work |
Why this step is crucial:
- Losing information increases abandonment rates & reduces repeat use
- When patients reach out via a channel for critical or emergent help, losing information when switching channels causes harmful delays
- The ability to transfer discussion between channels makes your services more adaptable when unforeseen situations arise (technology failure, local outbreak, spike in demand, etc.)
- Patients don’t like repeating themselves
Steps to take:
- Be sure the channels you have chosen (text chat, video chat, telephone, SMS, online forms, etc.) are all integrated
- Each channel should have access to the same or similar AI & clinical decision tools
- Staff should be trained on going back-&-forth between channels. This is easier if all channels are incorporated into a single interface
| Service platform facilitates all remote telehealth workflows |
Why this is crucial:
- In localized telehealth, the patient is remote but the service providers are all in a local location. Coordination is far easier when everyone is in the same place.
- In remote telehealth, the patient & the service providers are all remote. When this occurs, processes & collaboration tools must be well honed.
- Self-service improves patient satisfaction
- When telehealth staff can work remotely, your organization maximizes access & effectiveness when staff are immobilized, whether during extreme weather, local outbreaks, & more.
| Patient-reported & Cross-Channel KPI’s are captured |
Why this is crucial:
- Immediate & direct patient surveys are the best measure
- Cross channel KPI’s are needed for dem& management
Steps to take:
- Be sure all your channels (synchronous & asynchronous) report the following metrics:
- Satisfaction rating
- Custom patient surveys
- Channel preference by demographic, specialty, etc.
- Wait time per channel
- Outcomes & escalations per channel
OPTIMIZED
Summary
The Optimized stage builds on every prior stage. Providers can forecast demand, continuously improve service & quickly adjust workflows & processes in real time to changing circumstances. They are aware early of symptomatic trends across the population & have the tools & expertise in hand to direct dem& to the channels needed at the moment.
- Track symptomatic & syndromic trends in population
- Capture holistic patient experience KPI’s
- Forecast dem&
- Continuously measure & improve quality & efficiency of all channels
- Dem& management drives traffic to the most effective avenue
In Depth
| Track symptomatic & syndromic trends in population |
Why this step is crucial:
- Maximize service predictability
- React early to changes in your population
- Report key data to your public health board
Steps to take:
- Setup reporting & business intelligence to map address &/or zip code to symptomatic data
| Forecast demand |
Why forecasting is crucial:
- Reduce costs while maintaining quality
- Optimize workforce management
Steps to take:
- Build a forecast model from underlying cross-platform data
- Start with seasonality, & add trends, such as channel use, then modify for seasonal variations, such as timing of flu season
- With the right BI tool, this can be easily access in a dashboard at any time
| Continuously measure & improve quality & efficiency of all channels |
Why this step is crucial:
- Capture relative use, effectiveness, strengths, weaknesses, & outcomes of each channel for your local population
| Capture holistic patient experience KPI’s |
Why this step is crucial:.
- A few, simple service metrics yield the best correlation to behavior
- Closely monitoring these will yield optimized service delivery
Steps to take:
- Be sure all your channels (synchronous & asynchronous) report the following metrics:
- Net Promoter Score
- First contact resolution
- Customer Satisfaction Score
- Mean Time to Resolve
- Complaints
- For more information, see How to Grow 2x with the Right Scorecard
| Offer satisfaction guarantees for your telehealth services |
Why satisfaction guarantees are crucial:
- With deep knowledge of your service capabilities & adaptability, you can make a strong statement of assurance in your services
- Given your experience with adapting, the next unexpected event can be met with confidence
- Satisfaction guarantees have been closely linked to growth in a number of industries, especially if you have a first-mover advantage
Steps to take:
- Determine the target market for growth
- Determine the type of guarantee, the service guaranteed, the length of time, & how to evaluate conditions & process the benefits
- Advertise!
Posted By

Stephen Dean is COO of Keona Health, where he’s spent 13 years building AI systems that transform patient access. Before “agentic AI” was a term, his team was deploying autonomous systems that now handle millions of patient conversations annually.
Related Post
November 19, 2024
heading into 2025, healthcare organizations face increasing pressure to digitize...
October 18, 2023
is your healthcare call center getting crushed under the weight of frustrated...



