Telehealth has the tremendous potential of being faster and easier healthcare that improves patient access for all while improving provider revenue and flexibility.
That is not what most providers in 2020 have experienced. Telehealth satisfaction among providers has actually dropped! While a summary of studies in 2019 showed a majority of providers were satisfied with telemedicine (accessed Dec 12,2020), in 2020 only 26% of providers were satisfied (accessed Aug 20, 2020). Many providers experience telehealth as more frustrating, taking longer, and requiring more steps before, during, and after than traditional visits. Telehealth has turned out to be more complicated than providers were expecting.
Don't Take Your Eyes Off the Road!
It’s tempting for some to say, “It just doesn’t meet its potential,” but just because telehealth is more difficult than expected does not mean that it is not the best strategy. Healthcare has a lot as stake in making telehealth viable. Initial expectations on telehealth may have been missed, but once organizations understand the scope and needs of telehealth, the path to success becomes clear.
Keep reading for in-depth exploration of these themes along with a boatload of tips for getting past the complexity and improving telehealth.
The Surprising Breadth and Complexity of Telehealth
According to the U.S. Department of Health and Human Services (HHS) Telehealth is -
"Any use of electronic information and telecommunications technologies to support and promote long-distance clinical health care, patient and professional health-related education, and public health and health administration."
-Health Resources and Services Administration (HRSA)
This is far-reaching! Basically, any digital technology that provides services to patients over long-distance is part of telehealth.
This broad definition fits what we’ve seen in experience with COVID. An increase in telehealth has meant far more than an increase in video chats with a provider. It means
![]() Increases in telephone calls
Increases in telephone calls
![]() Increases in website visits
Increases in website visits
![]() More patient portal use
More patient portal use
 Increases to SMS (if available)
Increases to SMS (if available)
 Increases to video chat
Increases to video chat
This is just the front door! To be effective, delivery over telehealth requires a robust engine of workflow automation and the skilled driving of operations to support it! This means a holistic approach to telehealth is required.
Also see, A Digital Front Door is Grossly Inadequate.
Patient experience is fractured
If patients must take one set of actions to schedule an appointment, another to check in, and then a third thing for the video visit, a fourth to get the medication, and then a fifth to handle the payment, their experience is fractured.
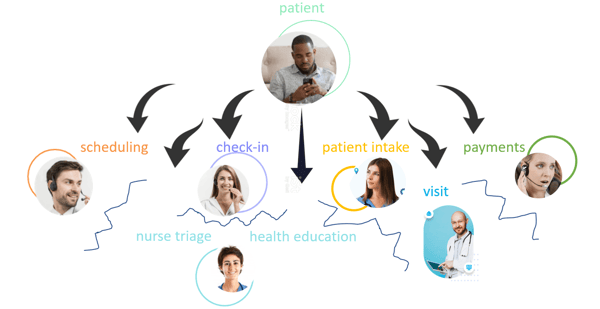
Provider experience is just as fractured
But it is not just the patient’s experience that is fractured. It is the health care provider’s experience that is even more fractured. There is not a smooth, holistic workflow that helps patients get what they need in a one-stop shop.
Why has provider satisfaction with telehealth fallen?
While there may be many reasons, a key one certainly has to be that telehealth is more complex and requires different skills. Keona Health has been publishing a series on telehealth skills.
 Then there is the urgency in which telehealth has been tackled. In their hurry to change during the COVID crisis, provider organizations had to jump on whatever technology was quickest to implement. This means it was often lacking EHR & PM integration, patient safety features, or even smooth scheduling and billing. That’s just the technology. The workflow innovation needed had to be figured out through trial and error. In other words, they were learning as they rushed forward. Many organizations were unprepared for the complexity or the demand they faced. The result is more work than expected by those involved and less revenue for the effort than expected.
Then there is the urgency in which telehealth has been tackled. In their hurry to change during the COVID crisis, provider organizations had to jump on whatever technology was quickest to implement. This means it was often lacking EHR & PM integration, patient safety features, or even smooth scheduling and billing. That’s just the technology. The workflow innovation needed had to be figured out through trial and error. In other words, they were learning as they rushed forward. Many organizations were unprepared for the complexity or the demand they faced. The result is more work than expected by those involved and less revenue for the effort than expected.
How to Race to Telehealth Success
As we move past the initial phases of COVID, many healthcare organizations will be looking to implement long-term telehealth solutions that are more permanent, are more integrated, offer automation, and doesn’t sidestep patient safety.
![]()
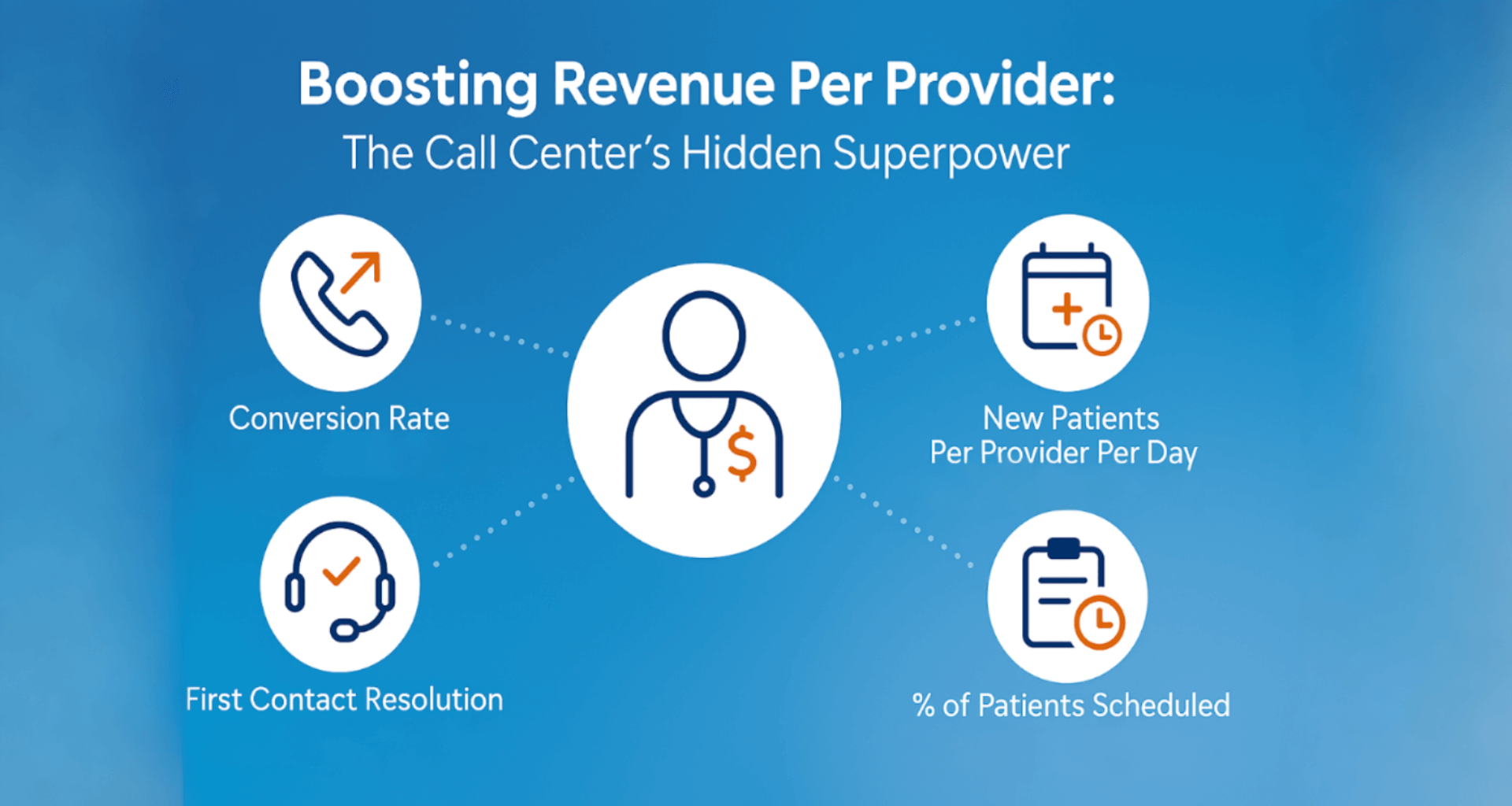
Break down silos & add automation in tandem with expanding telehealth
Most of the work needed to make telehealth a smooth experience for patients and providers is not on digital front-door technologies. Most of the work that needs to be done involves breaking down internal silos and automating services. These help make internal processes simpler, coordinated, and more agile.
Learn more about what is needed here in phase 2 (“Coordinated”) and 3 (“Automated”) of Keona’s Patient Service Maturity Model .
(see: https://www.getapp.com/resources/research-online-booking-importance-of-appointment-scheduling/
ECGMC.COM: https://bit.ly/39B9mxE
PatientGain: https://www.patientgain.com/patient-acquisition-vs-patient-retention)
This list of benefits seems tremendous. Why, then, hasn’t health care just adopted technology other industries already have to solve this?
The truth is, they have! The government subsidized the expansion of patient portals many years ago. Most patient portals have patient self-scheduling options. They are relatively unused.
Here are the problems they ran into
- Solutions required patients remember a login and password
With heavy promotion, patient portals will get substantial first-time use, but because a username and password is required and access is rare, they get far less repeat use - Once they login, they can’t schedule the appointment they need
Most providers and health systems only have a very short list of available appointments.
Usually the patient can only request an appointment and must wait on a scheduler to finalize - Patients put themselves in the wrong appointment all the time
these scheduling errors lead to communication burdens and patient safety issues
3 Barriers to self-scheduling
It turns out, healthcare scheduling has a few barriers that have been difficult to overcome.

Thankfully for the billions of online patients out there, each of these has a solution.
Login & Access
Like finance, healthcare is a regulated industry. Websites must meet government guidelines, notably HIPAA & HITECH. This has caused patient portals to require logins, just like your bank and credit card site. However, most consumers access their bank frequently. In this regard, the healthcare market is more like airlines, where there are a few frequent fliers but most people use only occasionally.

This raises another question. How do you schedule a healthcare appointment if the system doesn't know who you are or your health history?
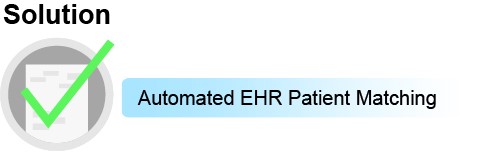
Automated EHR Patient Matching
By putting in just a few pieces of information, the patient can be matched against their record in the electronic health record or patient portal. A dashboard allows for quick review and approval for “maybe” matches.
Scheduling accuracy & available visit reasons
Scheduling accuracy is defined as the percentage of appointments that need to be rescheduled due to errors. For patient self-scheduling, “scheduling accuracy” refers to the tendency of patients to schedule the wrong appointment. Patients don’t know what types of visit are appropriate to their symptoms. Imagine trusting the patient to get the lab time right for testing, scheduling the right gap between that and the provider appointment, and figuring out the provider’s preferences for reviewing the results!
Even many people inside of healthcare aren’t aware of how complicated healthcare scheduling is. It causes a tremendous number of errors even for extensively trained and full-time schedulers. The power of combinatorics meant that just one mid-sized client of ours had over 50 million possible scheduling combinations! If you’re not familiar with these problems, we’ve written about the complexity problem of scheduling in this article. Go ahead and check it out, we’ll wait right here for you to come back:
The 3 Ways to Address Patient Scheduling Errors
The result of this complexity is that only a few visit reasons can be made available to patients. Nearly every patient portal allows patient self-scheduling, but typically only 3-7 visit reasons. This makes patient self-scheduling very limited. Patients usually request an appointment and wait for a scheduler to get back to them, which isn't very efficient or satisfying and doesn't even count as self-scheduling.
We pointed out that there are only 3 possible solutions to the complexity problem:
For patient self-scheduling, however, only 1 of these solutions solves scheduling accuracy and opens up the entire schedule for patient self-scheduling:
Scheduling Automation
Scheduling automation, like Care Desk Intelligent Scheduling, takes the complexity in scheduling and puts it into software. Because the computer system has been given the “training” for how to schedule, the patient doesn’t have to. It is so successful, clients of Intelligent Scheduling have gone from having 10% of their schedule online to having the entire scheduling calendar online, including complex imaging and surgeries!
While scheduling accuracy is the biggest benefit for Intelligent Patient Self-scheduling, it is by no means the only benefit. Other benefits are:
- Self-rescheduling: this scheduling automation allows patients to re-schedule themselves while keeping all the same scheduling rules and without re-asking all the questions that were asked the first time! This saves tremendous time on the part of the patients and your staff, and helps keep the schedule full.
- Automated Waitlist: waitlists give patients the chance for an earlier appointment if someone cancels. Let’s say your practice gets a reschedule for the next day. Self-scheduling waitlists matches that newly opened slot against all the criteria of patients in the waiting list, and offers to each patient in turn the opportunity to come in earlier and fill up that slot. Scheduling automation allows patients to opt-in to the waitlist, contacts patients in the waitlist when an opening becomes available, and lets patients update their phone numbers and manage their waitlist entries.
- Automate rescheduling campaigns: a provider gets sick and needs to reschedule all appointments for a day. A snow storm hits and an entire office has to reschedule every appointment for a day. With Patient self-scheduling it is easy to send every single patient an email or SMS message with an apology and a quick re-schedule link to find the next available appointment.
- Patient self-scheduling: helps patient navigate to where they need to go, electronically download or fill forms they need, or securely upload files.
Patient Safety
A patient schedules an appointment for a fever, headache and stiff neck. The next day they are in the ER with life-threatening meningitis that was totally preventable with earlier attention.
Situations like this keep providers and chief medical officers up at night.
There is an established process for patient safety in telehealth. It involves the following steps:
- Screen the patient for potentially dangerous symptoms (sometimes called “red flag list” or “symptom screening”)
- Based on the potential medical urgency of these symptoms, escalate the patient request
- This escalation is usually to a nurse
- If more urgent, it might involve paging a provider or even…
- Directing the patient to go to the emergency room or call 911
The problem with letting patients schedule themselves is that patients don’t know enough to appropriately screen their own symptoms. Few patients know that a stiff neck could be more than muscle strain, or even if they did, what additional questions they should be evaluating in order to remove that possibility. This is called, “triage” and nurses are licensed with special training to help patients through this.
Patient portals and even scheduling automation solutions haven’t found a solution, but one exists:
The power of natural language processing combined with specialty knowledge allows the following:
- Patient enters their symptoms just the way they would say it
- NLP associates their terms with clinical concepts
- The patient is asked a few clarifying questions
- The system directs them to schedule an appointment, talk to a nurse, or go the ER/call 911
This solution brings safety checks to the scheduling process in a way that gets patients to the help they need right away.
The vision of patient self-scheduling has been a pipedream for most organizations. Everyone wants it, but the barriers have been too hard to overcome. Thankfully, each of these has a proven safe and easy solution!
For more information, check out the following resources:
Patient Self-Scheduling
Natural Language Symptom Algorithms
Intelligent Scheduling
Ultimate Guide to Telehealth
About Keona Health
At Keona Health, we believe that relationships matter. We know that a clinic’s triage system can test a patient-doctor relationship, especially if a patient cannot easily get the help he or she is seeking. Keona Health offers healthcare software and automation solutions to ease the burden of telephone triage on medical practices and help medical professionals better communicate with patients.
Posted By

Stephen Dean is COO of Keona Health, where he’s spent 13 years building AI systems that transform patient access. Before “agentic AI” was a term, his team was deploying autonomous systems that now handle millions of patient conversations annually.
Related Post
July 30, 2025
when patients call, they’re not just dialing a number—they’re reaching for help. and...
April 10, 2025
in healthcare, every interaction is a decision point—one that can impact outcomes,...