Telehealth had a massive explosion in 2020 and by all accounts, it’s here to stay. However, surveys indicate that provider satisfaction has dropped precipitously. This is understandable when you consider how many organizations had to adopt the new technology very fast, underestimating the complexity of their own workflows. Unfortunately, this has resulted in more work for fewer visits.
We predict that 2021 will become the year of telehealth burnout – and even backlash. Learn more about these alarming trends and how to avoid them in your organization.
.png?width=92&name=SkyRocket%20(1).png) Telehealth skyrocketed in 2020
Telehealth skyrocketed in 2020
The amazing growth of telehealth is encapsulated in a single statistic: telehealth went from 2-3% of all visits in 2019 to 15-25% of all visits in 2020.
Frost & Sullivan research predicts a growth of nearly 20-25% in patient engagement management solutions in 2021. If so, telehealth usage will be 30-35% by the end of 2021
Patients love telehealth; 83% of patients who have used telemedicine in 2020 said they will continue to use it even after the COVID crisis is over.
.png?width=105&name=Burnout%20(1).png) Signs of burnout
Signs of burnout
But not so fast. Before the leaders get ahead of themselves, they need to take a closer look at what is happening on the front lines. That picture isn't as pretty.
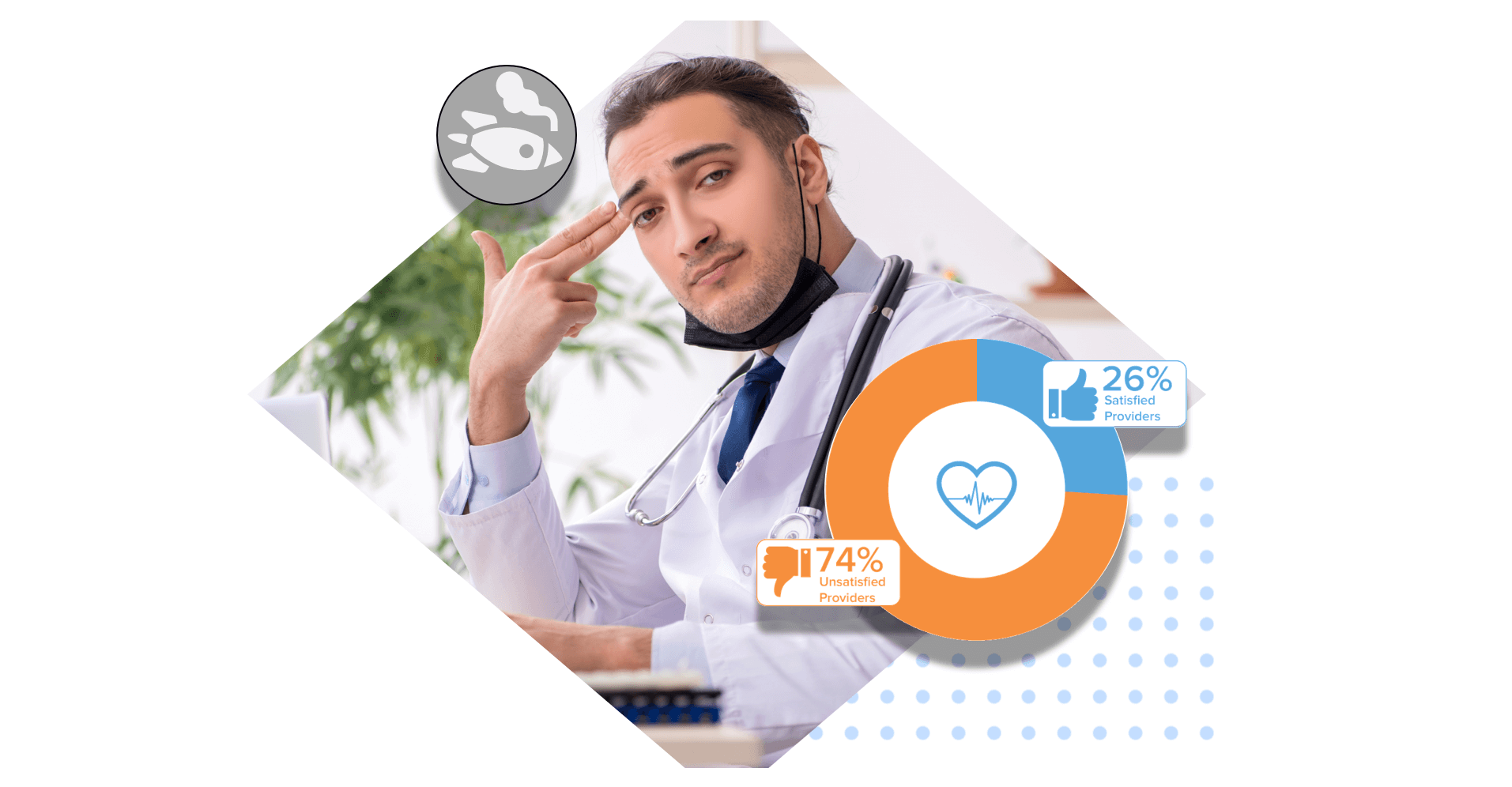
In 2019, studies showed a majority of providers were satisfied with telemedicine;
In 2020, only 26% of providers were satisfied.
While consultants and CEOs are bullish that 25-35% of visits will be telemedicine in 2021, providers are not; some 80% of physicians expect that telemedicine use will be under 10%.
Telehealth has turned out to be more complicated than providers were expecting. Many experience telehealth as more frustrating, taking longer, and requiring more steps.
While leaders will be focusing on building the most effective PR strategies to stay relevant, it will be years before healthcare develops the infrastructure to deliver on turnkey solutions. This exacerbates the burnout.
.png?width=92&name=Roles%20(1).png) Every role is affected
Every role is affected
The future of telehealth is likely in between those bullish on telehealth and those skeptical. In any case, telehealth is not going away. What's more, the recent move to telehealth has far-reaching implications across healthcare. Nearly every role inside provider organizations is facing increased work and complexity.
Clinic websites are getting more traffic
Telephone queues are more likely to be backed up
Scheduling changes happen more often
Workflow changes happen more often
Nurse triage guidelines change rapidly
Billing has new complexities and uncertainties.
This means that nearly every role within healthcare is affected, whether or not they are ever near a virtual visit themselves. Schedulers are affected, nurses are affected, billing is affected, contact center agents are affected.
 Symptoms of telehealth stress
Symptoms of telehealth stress
Do you see any of the following?
- Patients complaining about the telephone wait
- Providers complaining about telemedicine
- Staff social withdrawal
- Virtual visits drastically underperforming vs. in-person visits
- Providers, agents, and nurses complain about the extra documentation workload
- Patient requests and appointments are getting lost in the shuffle
- Drop in employee productivity
- Continuing to struggle with revenue
 Sources of telehealth stress
Sources of telehealth stress
- Burnout from the fast paced, surprising and complex nature of telehealth
- Burnout from rapid implementation
- Burnout from time management pressures
- Burnout from telemedicine
- Telephone volume burnout
- Scheduling changes burnout
 How to reduce telehealth stress
How to reduce telehealth stress
Not every organization faces the same level of burnout. From supporting staff to boning up on change management, here are things your organization can start today to make the move to telehealth easier on everyone.
Management Solutions
 1. Burnout from fast paced, surprising and complex nature of telehealth
1. Burnout from fast paced, surprising and complex nature of telehealth
Telehealth is more stressful and staff turnover is higher in telehealth roles. Most providers are familiar with fast-paced work, but telehealth adds even more stress. The inability to physically be with the patient add complexity. In addition, most telehealth workflows don’t give practitioners time to prepare for the visit; they have to figure out who they are talking to and what the issue is on-the-fly, compounding stress.
 Offer training in telehealth & emotional triggers
Offer training in telehealth & emotional triggers
Part of the reason that telehealth is more stressful is because both patients and staff are more blunt and easily irritated over electronic communications. Another is the fast-paced nature of telehealth. Prepare your staff for these with training and support. See some of our articles on telehealth training and management:
The Top 13 Patient Experience Metrics
See the Telehealth category in the Care Desk Blog for a wealth of training, tips, and strategy.
 Provide tools that reduce telehealth-related stress
Provide tools that reduce telehealth-related stress
- Step-by-step walkthroughsErrors are exacerbated when staff have high mental labor for each task - whether they are using many tools, looking up instructions, or cross-checking patient data in other windows. When you give staff tools that guide them through the steps needed without distraction, stress goes down and quality goes up.
- Make them aware of all services availableFew things are worse than a patient who needs help, but you don't have the tools you need. No one wants to hear, "Hang-up, call our main number again, but this time, hit option 2." Invest in the knowledge base, workflow, and scripting tools your staff needs to help patients the first time they call.
- Reduce the complexity of workflows with automationSometimes the problems are legitimately complex, and there is no way to reduce the stress except for automation. See The Only 3 Ways To Address Patient Scheduling Errors
- Consolidate workflows across traditional healthcare silosSee Patient Service Maturity Model
 2. Burnout from rapid implementation
2. Burnout from rapid implementation
A recent study found that 73% of change-affected employees report experiencing moderate-to-high levels of stress. This is why proper management is so crucial during the transition.
 Review best practices for change management
Review best practices for change management
As outlined by Smarp, a few key concepts are:defining clear goals;that everyone understands; building trust with honesty and transparency about the process encouraging communication; listening to your employees’ concerns; and implementing lots of training to help them get over the learning curve.
However, every organization is made out of people with differing personalities that can cause obstacles and/or resistance to change. Therefore it’s important to have an effective strategy to achieve your goals. But as article in the Harvard Business Review notes the most common mistake is to have a limited approach. It goes on to recommend tactics such as co-option – offering those that are resisting an important role in the process – as well as consistency with messaging that can help deal with any roadblocks.
 Be understanding about staff stress and initiate frequent dialogues
Be understanding about staff stress and initiate frequent dialogues
Employees who are dealing with depression or anxiety may be having difficulty feeling that they fit into the workplace. This also means they tend to withdraw or are silent about their issues, leading to a high level of turnover if not a general malaise. Therefore, you should do everything you can to bring to the surface discussions of what is going wrong and what can be done to improve the situation. Since this is healthcare, we are literally dealing with life-or-death situations and low morale can only make things worse.
 3. Burnout from time management pressures
3. Burnout from time management pressures
When change increases, it is incredibly hard not to fall into unrealistic expectations by leaders. Periods of relative stability allow for greater efficiency and perfection to be honed. In times of change, doing the same things that were done before result in less and less desirable outcomes. Prior levels of performance become harder and harder to maintain, which drives up stress.
 Involve front-line staff in architecting solutions
Involve front-line staff in architecting solutions
Research in telehealth indicates that workflows created with staff input are far more effective than ones created from top-down approaches, such as management design and consulting. Be sure to incorporate advocates from every role in the implementation process.
 Provide employees with rewards and incentives for problem solving
Provide employees with rewards and incentives for problem solving
Part of the solution is recognizing their efforts for solutions that help the entire organization.
 Expect less from staff
Expect less from staff
During times of rapid change, it takes more effort to accomplish the same workload. Nothing drives burnout faster than expecting even more. Greater productivity will be the eventual result of your investments in digital health, but don't expect it from day one!
 Use a management tool that measures telehealth demands in real-time
Use a management tool that measures telehealth demands in real-time
If you can’t measure the source of stress it will be more difficult to solve. That's why it's a good idea to invest in a healthcare CRM that can give you a holistic picture.
a. It can alert you when your appointments are starting to pile up
b. It can determine whether your appointments are running late
c. See trends in encounters that are lasting longer than normal
d. Pinpoint steps in the process that are causing backlogs
Operations Solutions
Operations solutions identify the largest sources of stress and modify the workflow accordingly.
 4. Burnout from telemedicine
4. Burnout from telemedicine
Telemedicine problems associated with burnout: Telemedicine tends to create more work than previously required. These are some of the problems adding to difficulties:
1. Less team support. Budget cuts at some facilities has made it difficult to maintain staff at optimum levels. This means more work for fewer people, leading to higher stress and quicker burnout.
2. Extra work. Virtual visits have added another layer of work to already burdened staff; some physicians now report spending half their day filling out EHR documentation.
3. Too many tools. It seems like every interaction is now in a separate app. Staff have to use the EHR for orders, visits via the telemedicine software, connect via secure VPN network, knowledge base through document management, coordinate with coworkers through text messenger, etc.
4. Lack of integration. When the rush to telemedicine occurred, many systems were quickly developed or implemented that are unable to connect. This has lead to duplicate tests, difficulty collaborating with other providers, and more time spent collecting external records.
5. Meeting documentation requirements. Compliance has been an essential part of patient services and is now even more complicated with telehealth and Covid. All patient paperwork must be secure, private, and accessible.
 Fully support practitioners in telemedicine visit
Fully support practitioners in telemedicine visit
The patient’s virtual visit should be just as quick and easy as in-person. Carefully planning the visit workflow is key. Consider the following to make it easier:
- Automate check-in OR have someone (not the practitioner) dedicated to patient check-ins
- Each patient to have their own “room” where staff cycles through to see them.
- Ability to centrally see all active “rooms” and monitor who is in each room, giving you a general overview of the entire process.
- Ability to review patient information and existing visit notes before entering the room, helping the provider quickly get up to speed without asking a lot of repetitive questions.
- Ability for care team and providers to leave and enter rooms as needed. Like a real office, practitioners need to move about in order to care for more patients efficiently.
- Ability to flag when a room is ready for the visit. The practitioner can quickly see where they need to appear next.
Having someone besides the practitioner check the patient in and review notes means that technical hurdles will usually be addressed before they show up.
If the connection is poor, both parties should turn off the camera unless/until needed. If the visit is reimbursable for audio only, there may be no reason to turn the cameras on at all.
 Make it easier with an integrated telemedicine solution
Make it easier with an integrated telemedicine solution
The more applications that staff must juggle, the more problems they have.
- more distractions
- more time each visit requires
- lower data quality
- higher burnout levels
You want a solution that automatically saves documentation to the EHR and integrates orders as well as allowing the practitioner to be able to do everything in one place easily with minimal distractions from the patient.
EHR integration from a web-based solution helps practitioners host visits while they are also remote or in areas where VPN isn’t available.
Many solutions tout EHR integration but don’t actually offer enough to make it valuable. Instead, the following integration features should be supported:
- Telemedicine scheduling
- Patient data directly from EHR
- Automated visit documentation written to EHR
- Read medications
- Orders placed through the EHR
 5. Telephone burnout
5. Telephone burnout
COVID has meant both more and longer phone calls, as patients need extra education and reassurance. This combination has been a double blow for practices not prepared for telehealth.
The problems associated with telephone burnout:
- Patients complaining about waiting in queue
- Operations can’t tell how big the backlog is or how long the wait
- Patient calls get lost in shuffle
- Lack of documentation on the call
- Longer phone calls
- Nursing documentation written hours later and/or skipped entirely
- Nurses are triaging on-the-fly without ready support
- Nurses are referencing the latest news they saw on social media
- Scheduling gaps go unfilled
Patients are upset if the nurse is unaware of what was said in the previous visit. If nurses are relaying inconsistent information or advice, patients lose trust. You need tools you don’t have in order to address these.
Solutions to Telephone Burnout
- Track every request and service provided – everyone can quickly see what was told to patients and when
- Speed up each call with a scripting tool that reduces the mental burden of telephone staff
- Improve service & reduce time with automated documentation – the scripting tool should auto-document the purpose of call and its outcome at the very minimum
- Triage software to lead nurses through best practice guidelines and auto-document the encounter
- A three-way integration between the telephone, scripting tool, and EHR will save another 30-50 seconds off each phone call
 6. Scheduling burnout
6. Scheduling burnout
COVID has thrown much of traditional scheduling out the window.
Scheduling problems that result are -
- The more schedules change, the more scheduling error
- Scheduling errors grow exponentially
- Organizations are faced with a tough choice
- Removing provider preferences and standardize scheduling
- Increase costs just to maintain scheduling efficiency
Solutions to scheduling
A. Centrally document all new scheduling requirements
B. Integrate scheduling into your telephone scripting tool
C. Automate scheduling to alleviate the mental burden, improve accuracy, and save time
D. Let patient schedule even complex visits themselves with patient self-scheduling
 MANAGE EVERYTHING WITH A HEALTHCARE CRM
MANAGE EVERYTHING WITH A HEALTHCARE CRM
Care Desk is a healthcare CRM and telehealth platform that provides a single place to implement all the workflow optimizations listed here. In this new era of digital health, a healthcare CRM will be just as important as your billing and EHR systems.
Reach out for a FREE consultation in how to address your burnout challenges.
.png?width=122&name=FastMoney%20(1).png) Act Fast – reimbursement may not last
Act Fast – reimbursement may not last
CMS is likely to reduce the rate for telehealth visits. It will be easier to tackle these barriers while CMS is still reimbursing telehealth.
Even while telemedicine is growing, hospital visits have remained flat. Therefore, the pressure to invest and reduce burnout is very high.
Ultimately, government action is needed to give the industry more time to adjust. If telehealth reimbursement is cut too soon, rural and vulnerable populations will be the hardest hit.
"Holding Providers Harmless From Medicare Cuts During COVID-19 Act of 2020" is a bill introduced by Representatives Dr. Ami Bera, D-Calif., and Dr. Larry Bucshon, R-Ind., that would temporarily maintain physicians' reimbursement in Medicare at 2020 levels for the next two years.
If reimbursement drops, the organizations who didn’t solve these problems will almost certainly de-prioritize telehealth as a strategic focus. On the other hand, organizations who addressed these issues will have long-term benefits, including increased patient access, longer growth, and better profit margins.
Contact Keona Health for your Telehealth consultation today.
For more information, check out the following resources:
About Keona Health
At Keona Health, we believe that relationships matter. We know that a clinic’s triage system can test a patient-doctor relationship, especially if a patient cannot easily get the help he or she is seeking. Keona Health offers healthcare software and automation solutions to ease the burden of telephone triage on medical practices and help medical professionals better communicate with patients.
Posted By

Stephen Dean is COO of Keona Health, where he’s spent 13 years building AI systems that transform patient access. Before “agentic AI” was a term, his team was deploying autonomous systems that now handle millions of patient conversations annually.
Related Post
November 19, 2024
heading into 2025, healthcare organizations face increasing pressure to digitize...
October 18, 2023
is your healthcare call center getting crushed under the weight of frustrated...



 Preventing Burnout
Preventing Burnout
